Sunday Poster Session
Category: Liver
P1153 - Non-Cirrhotic Hyperammonemia: A Rare Complication of Splenorenal Shunt Post Liver Transplant
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- NT
Nimish Thakral, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Nimish Thakral, MD1, Kishore Karri, MD1, Pradeep Yarra, MD, MSc2, Fady Salama, MD1, Kshitij Thakur, MD, MSc1
1University of Kentucky, Lexington, KY; 2Saint Louis University Hospital, St. Louis, MO
Introduction: Ammonia is a potent neurotoxin commonly implicated in the development of Hepatic Encephalopathy. While commonly associated with decompensated cirrhosis, hyperammonemia can be encountered in the absence of cirrhosis as well. Here we present a rare case of Hyperammonemic Encephalopathy (HE) in a patient with a remote history of liver transplant and intact liver function.
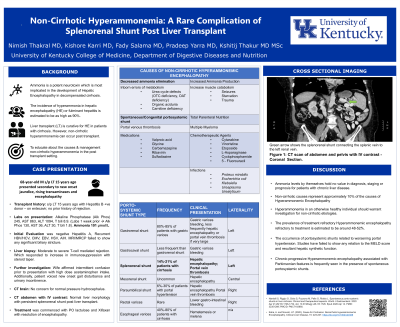
Case Description/Methods: A 69-year-old male with a history of remote liver transplant presented with new onset jaundice and fatigue. Initial lab work showed ALT 1094 IU/ml, AST 863 IU/ml, Total bilirubin 8.9 mg/dl, and Alkaline Phosphatase 245 IU/ml. Imaging did not show obstruction or vascular insult. EBV/CMV and HSV titers were negative. Subsequent liver biopsy showed severe T-cell-mediated rejection without significant fibrosis that responded to higher doses of immunosuppression and prednisone taper. Additionally, the patient's wife affirmed high dose Acetaminophen intake in the prior weeks with intermittent confusion. Given gait disturbances and long-standing history of urinary incontinence, the patient was initially thought to have normal pressure hydrocephalus. MRI brain however failed to show any corresponding changes. Furthermore, neuro-cognitive evaluation failed to show any cause of organic cause of neurological decline.
However, the initial lab work also showed hyperammonemia at 101 µmol/L. Subsequent CT abdomen with IV contrast showed the presence of a splenorenal shunt. On record review, the patient was found to have a persistent splenorenal shunt post-liver transplant. The patient responded well to treatment with lactulose and rifaximin with a decline in ammonia levels and no further episodes of encephalopathy.
Discussion: HE is a well-recognized complication of chronic liver disease (CLD) and is one of the defining features of decompensated cirrhosis. However, HE can also occur in the absence of CLD and present as new onset confusion or worsening mentation. Non-cirrhotic HE is usually seen in pediatric patients with disorders of urea cycle metabolism. In adults, however, the most common causes are increased muscle catabolism, infections, medications, and chemotherapeutic agents. In our patient, the cause was a persistent splenorenal shunt. Given that the patient responded well to medical treatment, invasive shunt closure was not attempted. Gastroenterologists must be aware of the causes of non-cirrhotic HE and have a high degree of suspicion in patients presenting with acute deterioration in mental status.
Disclosures:
Nimish Thakral, MD1, Kishore Karri, MD1, Pradeep Yarra, MD, MSc2, Fady Salama, MD1, Kshitij Thakur, MD, MSc1. P1153 - Non-Cirrhotic Hyperammonemia: A Rare Complication of Splenorenal Shunt Post Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2Saint Louis University Hospital, St. Louis, MO
Introduction: Ammonia is a potent neurotoxin commonly implicated in the development of Hepatic Encephalopathy. While commonly associated with decompensated cirrhosis, hyperammonemia can be encountered in the absence of cirrhosis as well. Here we present a rare case of Hyperammonemic Encephalopathy (HE) in a patient with a remote history of liver transplant and intact liver function.
Case Description/Methods: A 69-year-old male with a history of remote liver transplant presented with new onset jaundice and fatigue. Initial lab work showed ALT 1094 IU/ml, AST 863 IU/ml, Total bilirubin 8.9 mg/dl, and Alkaline Phosphatase 245 IU/ml. Imaging did not show obstruction or vascular insult. EBV/CMV and HSV titers were negative. Subsequent liver biopsy showed severe T-cell-mediated rejection without significant fibrosis that responded to higher doses of immunosuppression and prednisone taper. Additionally, the patient's wife affirmed high dose Acetaminophen intake in the prior weeks with intermittent confusion. Given gait disturbances and long-standing history of urinary incontinence, the patient was initially thought to have normal pressure hydrocephalus. MRI brain however failed to show any corresponding changes. Furthermore, neuro-cognitive evaluation failed to show any cause of organic cause of neurological decline.
However, the initial lab work also showed hyperammonemia at 101 µmol/L. Subsequent CT abdomen with IV contrast showed the presence of a splenorenal shunt. On record review, the patient was found to have a persistent splenorenal shunt post-liver transplant. The patient responded well to treatment with lactulose and rifaximin with a decline in ammonia levels and no further episodes of encephalopathy.
Discussion: HE is a well-recognized complication of chronic liver disease (CLD) and is one of the defining features of decompensated cirrhosis. However, HE can also occur in the absence of CLD and present as new onset confusion or worsening mentation. Non-cirrhotic HE is usually seen in pediatric patients with disorders of urea cycle metabolism. In adults, however, the most common causes are increased muscle catabolism, infections, medications, and chemotherapeutic agents. In our patient, the cause was a persistent splenorenal shunt. Given that the patient responded well to medical treatment, invasive shunt closure was not attempted. Gastroenterologists must be aware of the causes of non-cirrhotic HE and have a high degree of suspicion in patients presenting with acute deterioration in mental status.
Disclosures:
Nimish Thakral indicated no relevant financial relationships.
Kishore Karri indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Fady Salama indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Nimish Thakral, MD1, Kishore Karri, MD1, Pradeep Yarra, MD, MSc2, Fady Salama, MD1, Kshitij Thakur, MD, MSc1. P1153 - Non-Cirrhotic Hyperammonemia: A Rare Complication of Splenorenal Shunt Post Liver Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
