Sunday Poster Session
Category: Obesity
P1162 - Metabolic Healthy Obesity in Elderly Patients Hospitalized With Colorectal Cancer Showing Paradoxical Association With Composite in Hospital Outcomes: Insights from National Inpatient Sample 2019
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Mohammed Mustafa Nayeem, MD
Parkview Medical Center
Peublo, CO
Presenting Author(s)
Mohammed Mustafa Nayeem, MD1, Syed Mohammad Moosi Raza, MBBS2, Ali Tariq Alvi, MD3, Samridhi Lakhanpal, MBBS4, Thanmai Reddy Thugu, MBBS5, Siddharth Arjun. Atwal, MBBS6, Anusha Parisapogu, MBBS7, Sushrut Sarma Palepu, MBBS8, Masoud Amini, MD9, Trishna Acherjee, 10, Rupak Desai, MBBS11
1Parkview Medical Center, Peublo, CO; 2Fortis Escorts Heart Institute, New Delhi, Delhi, India; 3HCA Florida Westside Hospital, Plantation, FL; 4Saint Peter's University Hospital, New Brunswick, NJ; 5Sri Padmavathi Medical College for Women, SVIMS, Tirupathi, Andhra Pradesh, India; 6Civil Hospital Jalandhar, Jalandhar, Punjab, India; 7Mayo Clinic, Rochester, MN; 8Kasturba Medical College, Udupi, Karnataka, India; 9Mount Sinai Services-NYC Health+Hospitals/Queens, New York, NY; 10Reading Hospital Tower Health, Reading, PA; 11Outcomes Research, Atlanta, GA
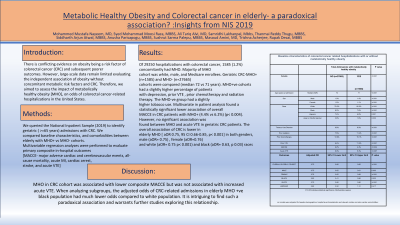
Introduction: There is conflicting evidence on obesity being a risk factor of colorectal cancer (CRC) and subsequent poorer outcomes. However, large-scale data remain limited evaluating the independent association of obesity without concomitant metabolic risk factors and CRC. Therefore, we aimed to assess the impact of metabolically healthy obesity [MHO], on odds of colorectal cancer-related hospitalizations in the United States.
Methods: We queried the National Inpatient Sample (2019) to identify geriatric ( >=65 years) admissions with CRC. We compared baseline characteristics, and comorbidities between elderly with MHO+ vs MHO- cohorts. Multivariable regression analyses were performed to evaluate primary composite in-hospital outcomes [MACCE- major adverse cardiac and cerebrovascular events, all-cause mortality, acute MI, cardiac arrest, stroke, and acute VTE]
Results: Of 29250 hospitalizations with colorectal cancer, 1585 (1.2%) concomitantly had MHO. Majority of MHO cohort was white, male, and Medicare enrollees. Geriatric CRC-MHO+ (n=1585) and MHO- (n=27665) cohorts were compared (median 72 vs 71 years). MHO+ve cohorts had a slightly higher percentage of patients with depression, prior VTE , prior chemotherapy and radiation therapy. The MHO-ve group had a slightly higher tobacco use. Multivariate in patient analysis found a statistically significant lower association of overall MACCE in CRC patients with MHO+ (4.4% vs 6.2%) (p< 0.004). However, no significant association was found between MHO and acute VTE in geriatric CRC patients. The overall association of CRC is lower in elderly MHO [ aOR 0.75, 95 CI 0.66-0.85, p< 0.001] in both genders, male (aOR= 0.75) , female (aOR=0.76) and white (aOR= 0.75 p< 0.001) and black (aOR= 0.63, p 0.03) races
Discussion: MHO in CRC cohort was associated with lower composite MACCE but was not associated with increased acute VTE. When analyzing subgroups, the adjusted odds of CRC-related admissions in elderly MHO +ve black population had much lower odds compared to white population. It is intriguing to find such a paradoxical association and warrants further studies exploring this relationship.
Disclosures:
Mohammed Mustafa Nayeem, MD1, Syed Mohammad Moosi Raza, MBBS2, Ali Tariq Alvi, MD3, Samridhi Lakhanpal, MBBS4, Thanmai Reddy Thugu, MBBS5, Siddharth Arjun. Atwal, MBBS6, Anusha Parisapogu, MBBS7, Sushrut Sarma Palepu, MBBS8, Masoud Amini, MD9, Trishna Acherjee, 10, Rupak Desai, MBBS11. P1162 - Metabolic Healthy Obesity in Elderly Patients Hospitalized With Colorectal Cancer Showing Paradoxical Association With Composite in Hospital Outcomes: Insights from National Inpatient Sample 2019, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Parkview Medical Center, Peublo, CO; 2Fortis Escorts Heart Institute, New Delhi, Delhi, India; 3HCA Florida Westside Hospital, Plantation, FL; 4Saint Peter's University Hospital, New Brunswick, NJ; 5Sri Padmavathi Medical College for Women, SVIMS, Tirupathi, Andhra Pradesh, India; 6Civil Hospital Jalandhar, Jalandhar, Punjab, India; 7Mayo Clinic, Rochester, MN; 8Kasturba Medical College, Udupi, Karnataka, India; 9Mount Sinai Services-NYC Health+Hospitals/Queens, New York, NY; 10Reading Hospital Tower Health, Reading, PA; 11Outcomes Research, Atlanta, GA
Introduction: There is conflicting evidence on obesity being a risk factor of colorectal cancer (CRC) and subsequent poorer outcomes. However, large-scale data remain limited evaluating the independent association of obesity without concomitant metabolic risk factors and CRC. Therefore, we aimed to assess the impact of metabolically healthy obesity [MHO], on odds of colorectal cancer-related hospitalizations in the United States.
Methods: We queried the National Inpatient Sample (2019) to identify geriatric ( >=65 years) admissions with CRC. We compared baseline characteristics, and comorbidities between elderly with MHO+ vs MHO- cohorts. Multivariable regression analyses were performed to evaluate primary composite in-hospital outcomes [MACCE- major adverse cardiac and cerebrovascular events, all-cause mortality, acute MI, cardiac arrest, stroke, and acute VTE]
Results: Of 29250 hospitalizations with colorectal cancer, 1585 (1.2%) concomitantly had MHO. Majority of MHO cohort was white, male, and Medicare enrollees. Geriatric CRC-MHO+ (n=1585) and MHO- (n=27665) cohorts were compared (median 72 vs 71 years). MHO+ve cohorts had a slightly higher percentage of patients with depression, prior VTE , prior chemotherapy and radiation therapy. The MHO-ve group had a slightly higher tobacco use. Multivariate in patient analysis found a statistically significant lower association of overall MACCE in CRC patients with MHO+ (4.4% vs 6.2%) (p< 0.004). However, no significant association was found between MHO and acute VTE in geriatric CRC patients. The overall association of CRC is lower in elderly MHO [ aOR 0.75, 95 CI 0.66-0.85, p< 0.001] in both genders, male (aOR= 0.75) , female (aOR=0.76) and white (aOR= 0.75 p< 0.001) and black (aOR= 0.63, p 0.03) races
Discussion: MHO in CRC cohort was associated with lower composite MACCE but was not associated with increased acute VTE. When analyzing subgroups, the adjusted odds of CRC-related admissions in elderly MHO +ve black population had much lower odds compared to white population. It is intriguing to find such a paradoxical association and warrants further studies exploring this relationship.
Table: Baseline patient characteristics and outcomes
Disclosures:
Mohammed Mustafa Nayeem indicated no relevant financial relationships.
Syed Mohammad Moosi Raza indicated no relevant financial relationships.
Ali Tariq Alvi indicated no relevant financial relationships.
Samridhi Lakhanpal indicated no relevant financial relationships.
Thanmai Reddy Thugu indicated no relevant financial relationships.
Siddharth Atwal indicated no relevant financial relationships.
Anusha Parisapogu indicated no relevant financial relationships.
Sushrut Sarma Palepu indicated no relevant financial relationships.
Masoud Amini indicated no relevant financial relationships.
Trishna Acherjee indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Mohammed Mustafa Nayeem, MD1, Syed Mohammad Moosi Raza, MBBS2, Ali Tariq Alvi, MD3, Samridhi Lakhanpal, MBBS4, Thanmai Reddy Thugu, MBBS5, Siddharth Arjun. Atwal, MBBS6, Anusha Parisapogu, MBBS7, Sushrut Sarma Palepu, MBBS8, Masoud Amini, MD9, Trishna Acherjee, 10, Rupak Desai, MBBS11. P1162 - Metabolic Healthy Obesity in Elderly Patients Hospitalized With Colorectal Cancer Showing Paradoxical Association With Composite in Hospital Outcomes: Insights from National Inpatient Sample 2019, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
