Sunday Poster Session
Category: Obesity
P1163 - Comparative Effectiveness of Surgical and Endoscopic Interventions in Obesity Management: A Network Meta-Analysis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Yianni Protopapadakis, MS, DO
Prisma Health System
Greenville, SC
Presenting Author(s)
Yianni Protopapadakis, MS, DO1, Kalpit Devani, MD2, Dhruvil Radadiya, MD3, Lauryn Hutto, MS1, Jena Velji-Ibrahim, MD1
1Prisma Health System, Greenville, SC; 2Prisma Health Upstate, Greenville, SC; 3University of Kansas Medical Center, Kansas City, KS
Introduction: Obesity is a global health issue of epidemic proportions. Surgical interventions have traditionally served as the standard of care for managing obesity. However, the past decade has witnessed a surge in the development and utilization of endoscopic interventions for obesity management, broadening the range of available treatments. Despite these advancements, the comparative evidence between surgical and endoscopic procedures is insufficient.
Methods: We systematically searched electronic databases for randomized controlled trials (RCTs) evaluating the comparing efficacy of surgical and endoscopic interventions for obesity management. We extracted percentage weight loss (mean and SD). A network meta-analysis using frequentist methods with a random-effect model was conducted. The p-score was calculated to obtain treatment ranking to identify preferred intervention to achieve maximal percentage reduction in weight change. A league table provided network estimates of each possible comparison of surgical and endoscopic interventions.
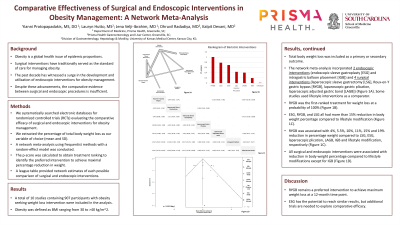
Results: A total of 10 studies comprising 907 participants with obesity (defined as BMI ranging from 30 to >40 kg/m^2) seeking weight loss intervention were included in the analysis. Total body weight loss was included as a primary or secondary outcome. The network meta-analysis incorporated 2 endoscopic interventions (Endoscopic Sleeve Gastroplasty [ESG] and Intragastric balloon placement [IGB]) and 4 surgical interventions (Laparoscopic sleeve gastrectomy [LSG], Roux-en-Y gastric bypass [RYGB], laparoscopic plication, laparoscopic adjusted gastric band [LAGB]) with some studies using lifestyle interventions as comparator (Figure 1A). RYGB was associated with 4%, 5.5%, 10%, 11%, 15% and 19% reduction in percentage weight compared to LSG, ESG, laparoscopic plication, LAGB, IGB and lifestyle modification (Figure 1B). ESG, RYGB, and LSG all had more than 15% reduction in body weight percentage compared to lifestyle modification (Figure 1B). RYGB was the first-ranked treatment for weight loss at a probability of 100% (Figure 1C). On network comparison with placebo, all surgical and endoscopic interventions were associated with reduction in body weight percentage compared to lifestyle modifications except for IGB (Figure 1D).
Discussion: RYGB remains a preferred intervention to achieve maximum weight loss at a 12-month time point. ESG has the potential to reach similar results, but additional trials are needed to explore comparative efficacy.

Disclosures:
Yianni Protopapadakis, MS, DO1, Kalpit Devani, MD2, Dhruvil Radadiya, MD3, Lauryn Hutto, MS1, Jena Velji-Ibrahim, MD1. P1163 - Comparative Effectiveness of Surgical and Endoscopic Interventions in Obesity Management: A Network Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Prisma Health System, Greenville, SC; 2Prisma Health Upstate, Greenville, SC; 3University of Kansas Medical Center, Kansas City, KS
Introduction: Obesity is a global health issue of epidemic proportions. Surgical interventions have traditionally served as the standard of care for managing obesity. However, the past decade has witnessed a surge in the development and utilization of endoscopic interventions for obesity management, broadening the range of available treatments. Despite these advancements, the comparative evidence between surgical and endoscopic procedures is insufficient.
Methods: We systematically searched electronic databases for randomized controlled trials (RCTs) evaluating the comparing efficacy of surgical and endoscopic interventions for obesity management. We extracted percentage weight loss (mean and SD). A network meta-analysis using frequentist methods with a random-effect model was conducted. The p-score was calculated to obtain treatment ranking to identify preferred intervention to achieve maximal percentage reduction in weight change. A league table provided network estimates of each possible comparison of surgical and endoscopic interventions.
Results: A total of 10 studies comprising 907 participants with obesity (defined as BMI ranging from 30 to >40 kg/m^2) seeking weight loss intervention were included in the analysis. Total body weight loss was included as a primary or secondary outcome. The network meta-analysis incorporated 2 endoscopic interventions (Endoscopic Sleeve Gastroplasty [ESG] and Intragastric balloon placement [IGB]) and 4 surgical interventions (Laparoscopic sleeve gastrectomy [LSG], Roux-en-Y gastric bypass [RYGB], laparoscopic plication, laparoscopic adjusted gastric band [LAGB]) with some studies using lifestyle interventions as comparator (Figure 1A). RYGB was associated with 4%, 5.5%, 10%, 11%, 15% and 19% reduction in percentage weight compared to LSG, ESG, laparoscopic plication, LAGB, IGB and lifestyle modification (Figure 1B). ESG, RYGB, and LSG all had more than 15% reduction in body weight percentage compared to lifestyle modification (Figure 1B). RYGB was the first-ranked treatment for weight loss at a probability of 100% (Figure 1C). On network comparison with placebo, all surgical and endoscopic interventions were associated with reduction in body weight percentage compared to lifestyle modifications except for IGB (Figure 1D).
Discussion: RYGB remains a preferred intervention to achieve maximum weight loss at a 12-month time point. ESG has the potential to reach similar results, but additional trials are needed to explore comparative efficacy.

Figure: Figure 1A: Network graph demonstrating the comparisons made between the included intervention types.
Figure 1B: League table (pairwise comparisons) of the evaluated bariatric interventions (demonstrated as relative effect and [95% Credible Interval]).
Figure 1C: Ranking of weight-loss interventions based on p-score.
Figure 1D: Forest Plot (random effects model) comparing weight changes in the examined weight-loss interventions versus 'lifestyle changes'.
Figure 1B: League table (pairwise comparisons) of the evaluated bariatric interventions (demonstrated as relative effect and [95% Credible Interval]).
Figure 1C: Ranking of weight-loss interventions based on p-score.
Figure 1D: Forest Plot (random effects model) comparing weight changes in the examined weight-loss interventions versus 'lifestyle changes'.
Disclosures:
Yianni Protopapadakis indicated no relevant financial relationships.
Kalpit Devani indicated no relevant financial relationships.
Dhruvil Radadiya indicated no relevant financial relationships.
Lauryn Hutto indicated no relevant financial relationships.
Jena Velji-Ibrahim indicated no relevant financial relationships.
Yianni Protopapadakis, MS, DO1, Kalpit Devani, MD2, Dhruvil Radadiya, MD3, Lauryn Hutto, MS1, Jena Velji-Ibrahim, MD1. P1163 - Comparative Effectiveness of Surgical and Endoscopic Interventions in Obesity Management: A Network Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
