Sunday Poster Session
Category: Liver
P0946 - Effects of Paracentesis Timing and Service on Length of Stay
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Tianyu She, DO
NYU Long Island
Mineola, NY
Presenting Author(s)
Tianyu She, DO, Nathan Starkman, MD, Bharat Hans, MD, MSc, Meredith Akerman, MS, Aleksey Etinger, DO
NYU Long Island, Mineola, NY
Introduction: Diagnostic paracentesis has long been known to be critical in the management of decompensated cirrhosis. Additionally, it has been established that earlier inpatient paracentesis is associated with fewer complications, lower in-hospital mortality, and shorter length of stay (LOS). With recent creation of a non-dedicated hospitalist paracentesis team, we analyzed time elapsed to paracentesis (TEP) in relation to the different services of interventional radiology (IR), medicine teams, and the emergency department (ED) and its effect on LOS in our institution.
Methods: All inpatient medicine and subspecialty admissions with ascites requiring paracentesis ranging from 01/2021-05/2023 were queried. Palliative, deceased, outpatient, and subsequent paracentesis within the same admission were excluded. We separated the TEP to 0 (< 24 hours, same day of admission), 1 (24-48 hours) , or 2+ ( > 48 hours) days, recorded the performing department, and LOS. Additionally, we compared the data before and after 01/2022, which represents the establishment of the non-dedicated hospitalist paracentesis team. Spearman coefficients were used to assess the association between TEP and LOS. The Mann-Whitney test or Kruskal-Wallis test was used to compare non-normally distributed continuous data between groups. A result was significant at p< 0.05.
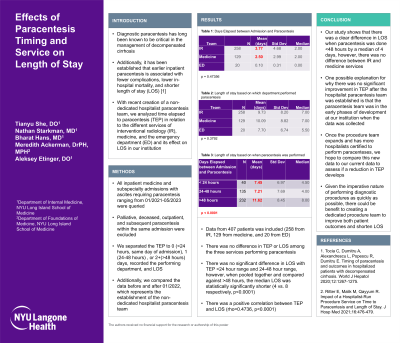
Results: Data from 407 patients was included (258 from IR, 129 from medicine, and 20 from ED). There was a positive correlation between TEP and LOS (rho=0.4736, p< 0.0001). There was no significant difference in LOS with TEP < 24 hour range and 24-48 hour range, however, when pooled together and compared against > 48 hours, the median LOS was statistically significantly shorter (4 vs. 8 respectively, p< 0.0001 (Fig. 1)). There was no difference in LOS among the three services performing paracentesis. The median TEP was 2 days for both IR and medicine services. There was not a significant difference in median LOS before and after 01/2022 (7 vs. 7.5 days respectively, significant=0.4009).
Discussion: Our study shows that there was a clear difference in LOS when paracentesis was done < 48 hours by a median of 4 days, however, there was no difference between IR and medicine services. Studies have demonstrated that a dedicated procedure service is associated with shorter LOS. Given the imperative nature of performing diagnostic procedures as quickly as possible, there could be benefit to creating a dedicated procedure team to improve both patient outcomes and shorten LOS.

Disclosures:
Tianyu She, DO, Nathan Starkman, MD, Bharat Hans, MD, MSc, Meredith Akerman, MS, Aleksey Etinger, DO. P0946 - Effects of Paracentesis Timing and Service on Length of Stay, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
NYU Long Island, Mineola, NY
Introduction: Diagnostic paracentesis has long been known to be critical in the management of decompensated cirrhosis. Additionally, it has been established that earlier inpatient paracentesis is associated with fewer complications, lower in-hospital mortality, and shorter length of stay (LOS). With recent creation of a non-dedicated hospitalist paracentesis team, we analyzed time elapsed to paracentesis (TEP) in relation to the different services of interventional radiology (IR), medicine teams, and the emergency department (ED) and its effect on LOS in our institution.
Methods: All inpatient medicine and subspecialty admissions with ascites requiring paracentesis ranging from 01/2021-05/2023 were queried. Palliative, deceased, outpatient, and subsequent paracentesis within the same admission were excluded. We separated the TEP to 0 (< 24 hours, same day of admission), 1 (24-48 hours) , or 2+ ( > 48 hours) days, recorded the performing department, and LOS. Additionally, we compared the data before and after 01/2022, which represents the establishment of the non-dedicated hospitalist paracentesis team. Spearman coefficients were used to assess the association between TEP and LOS. The Mann-Whitney test or Kruskal-Wallis test was used to compare non-normally distributed continuous data between groups. A result was significant at p< 0.05.
Results: Data from 407 patients was included (258 from IR, 129 from medicine, and 20 from ED). There was a positive correlation between TEP and LOS (rho=0.4736, p< 0.0001). There was no significant difference in LOS with TEP < 24 hour range and 24-48 hour range, however, when pooled together and compared against > 48 hours, the median LOS was statistically significantly shorter (4 vs. 8 respectively, p< 0.0001 (Fig. 1)). There was no difference in LOS among the three services performing paracentesis. The median TEP was 2 days for both IR and medicine services. There was not a significant difference in median LOS before and after 01/2022 (7 vs. 7.5 days respectively, significant=0.4009).
Discussion: Our study shows that there was a clear difference in LOS when paracentesis was done < 48 hours by a median of 4 days, however, there was no difference between IR and medicine services. Studies have demonstrated that a dedicated procedure service is associated with shorter LOS. Given the imperative nature of performing diagnostic procedures as quickly as possible, there could be benefit to creating a dedicated procedure team to improve both patient outcomes and shorten LOS.

Figure: Figure 1. Distribution of length of stay for paracentesis within 48 hours resulting in a median reduction of four days.
Disclosures:
Tianyu She indicated no relevant financial relationships.
Nathan Starkman indicated no relevant financial relationships.
Bharat Hans indicated no relevant financial relationships.
Meredith Akerman indicated no relevant financial relationships.
Aleksey Etinger indicated no relevant financial relationships.
Tianyu She, DO, Nathan Starkman, MD, Bharat Hans, MD, MSc, Meredith Akerman, MS, Aleksey Etinger, DO. P0946 - Effects of Paracentesis Timing and Service on Length of Stay, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
