Sunday Poster Session
Category: Liver
P0957 - Palliative Care Is Underutilized in Patients with Cirrhosis Admitted to the Intensive Care Unit Observations from a Large Academic Transplant Center

Jonathan Montrose, DO
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Jonathan Montrose, DO1, Jessica Adams, MD2, Michael Rosenheck, MD1, Jennifer Peng, MD3, Archita Desai, MD3, Lauren Nephew, MD3, Eric Orman, MD3, Marwan Ghabril, MD3, Kavish Patidar, MD4, Amy Johnson, DO1
1Indiana University School of Medicine, Indianapolis, IN; 2IU School of Medicine, Indianapolis, IN; 3Indiana University, Indianapolis, IN; 4Baylor College of Medicine, Houston, TX
Introduction: In patients with cirrhosis once there are signs of clinical decompensation there is a significant decline in quality of life and life expectancy. This creates the opportunity for high quality palliative care (PC) along with goals of care (GOC) conversations and advanced care planning.
Methods: Retrospective cohort study of individuals with cirrhosis admitted to the ICU at two large referral centers. Appropriate ICD-10 codes for cirrhosis were used to screen patients with an ICU admission from 1/1/2016-12/31/2019 and confirmed through chart review. Primary outcome examined the frequency of GOC conversations and the impact on patient outcomes.
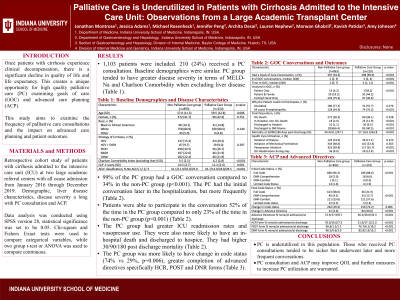
Results: Of the 1,103 patients included, only 210 (24%) received a PC consultation. The mean age, percent female and etiology of cirrhosis was similar. The PC group had a higher mean Charlson Comorbidity Index (3.5 vs 4.2, p< 0.001), CLIF-C score (10.5 vs 11.2, p=0.001), ACLF classification ≥2 (42% vs 54%, p< 0.001), and MELD-Na (24 vs 28, p< 0.001). In the PC group, 99% had a GOC conversation compared to 34% of the non-PC group (p< 0.001). The PC group had initial GOC conversation sooner with a median time of 2 days, and more often with a median of 3 conversations compared to 4 days (p< 0.001) and 2 conversations (p< 0.001) in the non-PC. Patients were able to participate 52% of the time in the PC group compared to 23% in the non-PC (p< 0.001). 75% of the PC group had a change in code status compared to 30% of the non-PC (p=0.006). Advanced directives were completed 40% of the time in the PC group compared to 4.6% in the non-PC group (p< 0.001) with greater completion rates of health care representative forms (33%), POST forms (16%) and DNR forms (15%) prior to discharge compared to the non-PC group at 8%, 1% and 2%, respectively (p< 0.001).There was no difference in initiation of dialysis or mechanical ventilation, but the PC group had greater vasopressor initiation (56%) and ICU readmissions (12%) compared to the non-PC group at 40% and 4%, respectively (p< 0.001). The PC group experienced more ICU death (38%), in-hospital non-ICU death (12%) and hospice placement (10%) compared to 35% (p=0.028), 2%, and 1%, respectively (p< 0.001). There was higher mortality at 30,90, and 180-days (p< 0.001) in the PC group.
Discussion: While PC remains underutilized, those who received a PC consultation tended to be sicker and underwent earlier and more frequent GOC conversations. Further measures to increase PC utilization in this population is warranted.
Characteristic | Non-Palliative Care group (n=893) | Palliative Care Group (n=210) | p-value |
Age (SD) | 57.0 (11.3) | 59.5 (12.8) | 0.006 |
Female, n (%) | 372 (41.7) | 90 (42.9) | 0.751 |
Race, n (%) Black or African American White Other |
90 (10.1) 758 (84.9) 45 (5.0) |
31 (14.8) 169 (80.5) 0 (4.8) |
0.140 |
Insurance, n (%) Commercial Medicaid Medicare Other |
6 (0.7) 295 (33.0) 382 (42.8) 210 (23.5) |
1 (0.5) 67 (31.9) 109 (51.9) 33 (15.7) |
0.045 |
Etiology of Cirrhosis, n (%) HCV HCV + EtOH EtOH NASH Other |
137 (15.3) 87 (9.7) 290 (32.5) 197 (22.0) 182 (22.4) |
43 (20.5) 19 (9.0) 56 (26.7) 46 (21.9) 46 (21.9) |
0.297 |
Charlson Comorbidity Index (excluding liver) (SD) | 3.5 (2.5) | 4.2 (2.8) | < 0.001 |
CLIF-C score (SD) | 10.5 (2.7) | 11.2 (2.4) | 0.001 |
ACLF classification, % No ACLF/ 1/ 2/ 3 | 31.1/11.9/16.9/25.0 | 16.7/12.9/24.8/29.5 | < 0.001 |
Initial MELD-Na (SD) | 24.1 (10.4) | 27.8 (9.8) | < 0.001 |
Initial Code Status, n (%) Full Code DNR-Comprehensive DNR-Comfort Limited Code Status |
860 (96.3) 18 (2.0) 1 (0.1) 14 (1.6) |
186 (88.6) 18 (8.6) 0 (0.0) 4 (1.9) |
< 0.001 |
Final Code Status, n (%) Full Code DNR-Comprehensive DNR-Comfort Limited Code status |
613 (68.6) 40 (4.5) 211 (23.6) 22 (2.5) |
46 (21.9) 33 (15.7) 121 (57.6) 5 (2.4) |
< 0.001 |
Change in Code status | 262 (29.3) | 156 (74.2) | 0.006 |
Change in Advance Directive | 41 (4.6) | 84 (40.0) | < 0.001 |
Advance Directives % none/at admission/at discharge | 72.9/17.9/8.7 | 36.2/30.0/33.3 | < 0.001 |
HCR Form % none/at admission/at discharge | 76.0/16.0/7.5 | 51.9/27.1/21.0 | < 0.001 |
POST Form % none/at admission/at discharge | 96.8/1.2/1.1 | 76.7/6.2/16.2 | < 0.001 |
DNR Form % none/at admission/at discharge | 96.5/0.6/2.0 | 82.8/1.9/15.2 | < 0.001 |
Health Care Utilization, n (%) Initiation of Dialysis Required Mechanical Ventilation Vasopressor use ICU Readmission during stay |
125 (14.0) 343 (48.6) 355 (39.8) 36 (4.0) |
36 (17.1) 110 (52.4) 117 (55.7) 26 (12.4) |
0.573 0.563 < 0.001 < 0.001 |
Had a Goals of Care Conversation, n (%) | 307 (34.4) | 208 (99.0) | < 0.001 |
# of GOC conversations, median (IQR) | 2 (2, 3) | 3 (2, 4) | < 0.001 |
Time to GOC, median (IQR) | 2 (0, 7) | 4 (1, 11) | < 0.001 |
Trigger for GOC, n (%) Upgrade to ICU Bleed Change in Respiratory Status Need for Dialysis Hypotension/Vasopressor need Primary Team Requested Family Requested Not a Liver Transplant Candidate Other |
90 (10.1) 61 (6.8) 118 (13.2) 46 (5.2) 163 (18.3) 67 (7.5) 20 (2.2) 10 (1.1) 100 (11.2) |
37 (17.6) 29 (13.8) 54 (25.7) 33 (15.7) 68 (32.4) 84 (40.0) 16 (7.6) 31 (14.8) 76 (36.2) |
0.002 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 |
Involved in GOC, n (%) Patient Only Patient & Family Family/Friend Only |
13 (4.2) 59 (19.2) 233 (75.9) |
17(8.2) 92 (44.2) 97 (46.6) |
< 0.001 |
Why the Patient could not Participate, n (%) Intubated Metabolic Encephalopathy |
180 (77.3) 128 (54.9) |
54 (55.7) 74 (76.3) |
0.076 < 0.001 |
Final Disposition, n (%) ICU Death In-Hospital, non-ICU Death Discharged to Hospice Discharged to SNF/Home |
272 (30.5) 18 (2.0) 10 (1.1) 593(66.4) |
80 (38.1) 25 (11.9) 20 (9.5) 85 (40.5) |
0.028 < 0.001 < 0.001 < 0.001 |
Mortality at 30/90/180 days Post-Discharge (%) | 34.4/41.2/47.1 | 57.1/61.0/63.8 | < 0.001 |
Liver Transplant Status, n (%) Evaluated for Transplant Listed for Transplant Received Transplant |
110 (12.3) 83 (9.3) 66 (7.4) |
12 (5.7) 0 (0) 0(0) |
0.005 < 0.001 < 0.001 |
Disclosures:
Jonathan Montrose, DO1, Jessica Adams, MD2, Michael Rosenheck, MD1, Jennifer Peng, MD3, Archita Desai, MD3, Lauren Nephew, MD3, Eric Orman, MD3, Marwan Ghabril, MD3, Kavish Patidar, MD4, Amy Johnson, DO1. P0957 - Palliative Care Is Underutilized in Patients with Cirrhosis Admitted to the Intensive Care Unit Observations from a Large Academic Transplant Center, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

