Sunday Poster Session
Category: Liver
P0962 - Ethnic and Racial Disparities in Alcoholic Liver Disease Related Mortality: Data From CDC Wonder 1999-2020
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Fariha Ilyas, MD
ECU Health Medical Center / Brody School of Medicine
Greenville, NC
Presenting Author(s)
Fariha Ilyas, MD1, Hassam Ali, MD1, Stephanie Ibarra, MD1, Pratik Patel, MD2, Alexa Giammarino, MD3, Sanjaya Satapathy, MD3
1ECU Health Medical Center / Brody School of Medicine, Greenville, NC; 2Mather Hospital/Hofstra University Zucker School of Medicine, Port Jefferson, NY; 3North Shore University Hospital/Zucker School of Medicine at Hofstra University, Manhasset, NY
Introduction: Alcoholic liver disease (ALD) has significant morbidity and mortality in adults. With evolving trends in prevalence of liver pathologies, we aimed to stratify mortality trends of ALD based on race/ethnicity in the United States from 1999-2020.
Methods: We used CDC Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) to access National Vital Statistics System data from 1999-2020. ALD related deaths in adults with age 25-85+ years were identified. Deaths were shown as age adjusted mortality rates (AAMR) per 100,000 population. Joinpoint regression was used to examine changes in trend, average annual percent change (AAPC) and annual percentage change (APC) in ALD related deaths, stratified by racial/ethnic groups [Whites, African Americans (AA), Hispanics, Asian or Pacific Islanders (API) and American Indians or Alaska Natives (AI/AN)].
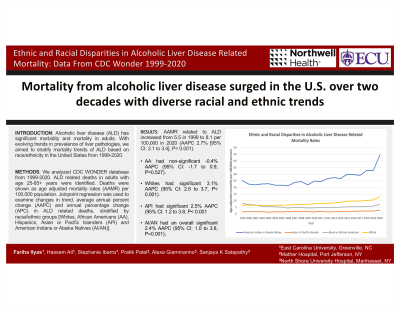
Results: AAMR related to ALD increased from 5.5/100,000 in 1999 to 8.1/100,000 in 2020 (AAPC 2.7% [95% CI: 2.1 to 3.4], P< 0.001). AA had an overall non-significant -0.4% AAPC (95% CI: -1.7 to 0.9, P=0.527). There was significant decrease in 1999-2006 (APC: -7.1%, 95% CI: -8.7 to -5.5, P< 0.001), increase in 2006-2018 (APC: 1.6%, 95% CI: 0.7 to 2.5, P=0.002), and non-significant increase in 2018-2020 (APC: 12.9%, 95% CI: -0.7 to 28.5, P=0.063). Whites had an overall significant 3.1% AAPC (95% CI: 2.6 to 3.7, P< 0.001). There was no significant change in 1999-2005 (APC: -0.2%, 95% CI: -1.2 to 0.7, P=0.618), but significant increases were seen in 2005-2018 (APC: 3.5%, 95% CI: 3.1 to 3.8%, P< 0.001) and 2018-2020 (APC: 11.6%, 95% CI: 5.5 to 18.1, P=0.001). API had an overall significant 2.5% AAPC (95% CI: 1.2 to 3.8, P< 0.001); no significant increase seen in 1999-2013 (APC: 0.5%, 95% CI: -0.7 to 1.7%, P=0.409) but a significant increase in 2013-2020 was observed (APC: 6.6%, 95% CI: 3.1 to 10.3%, P=0.001). AI/AN had an overall significant 2.4% AAPC (95% CI: 1.0 to 3.8, P=0.001); non-significant decrease in 1999-2005 (APC: -1.7%, 95% CI: -3.8 to 0.6, P=0.129), significant increase in 2005-2018 (APC: 2.7%, 95% CI: 1.9 to 3.5%, P< 0.001) and a non-significant increase in 2018-2020 (APC: 13.4%, 95% CI: -0.7 to 29.4, P=0.062).
Discussion: From 1999-2020, mortality in ALD increased, with trends varying among races/ethnicities: AA displayed a non-significant overall trend, while Whites, API, and AI/AN showed significant increase with varied segments. ALD mortality remains a critical public health concern, with notable differences across demographics.

Disclosures:
Fariha Ilyas, MD1, Hassam Ali, MD1, Stephanie Ibarra, MD1, Pratik Patel, MD2, Alexa Giammarino, MD3, Sanjaya Satapathy, MD3. P0962 - Ethnic and Racial Disparities in Alcoholic Liver Disease Related Mortality: Data From CDC Wonder 1999-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1ECU Health Medical Center / Brody School of Medicine, Greenville, NC; 2Mather Hospital/Hofstra University Zucker School of Medicine, Port Jefferson, NY; 3North Shore University Hospital/Zucker School of Medicine at Hofstra University, Manhasset, NY
Introduction: Alcoholic liver disease (ALD) has significant morbidity and mortality in adults. With evolving trends in prevalence of liver pathologies, we aimed to stratify mortality trends of ALD based on race/ethnicity in the United States from 1999-2020.
Methods: We used CDC Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) to access National Vital Statistics System data from 1999-2020. ALD related deaths in adults with age 25-85+ years were identified. Deaths were shown as age adjusted mortality rates (AAMR) per 100,000 population. Joinpoint regression was used to examine changes in trend, average annual percent change (AAPC) and annual percentage change (APC) in ALD related deaths, stratified by racial/ethnic groups [Whites, African Americans (AA), Hispanics, Asian or Pacific Islanders (API) and American Indians or Alaska Natives (AI/AN)].
Results: AAMR related to ALD increased from 5.5/100,000 in 1999 to 8.1/100,000 in 2020 (AAPC 2.7% [95% CI: 2.1 to 3.4], P< 0.001). AA had an overall non-significant -0.4% AAPC (95% CI: -1.7 to 0.9, P=0.527). There was significant decrease in 1999-2006 (APC: -7.1%, 95% CI: -8.7 to -5.5, P< 0.001), increase in 2006-2018 (APC: 1.6%, 95% CI: 0.7 to 2.5, P=0.002), and non-significant increase in 2018-2020 (APC: 12.9%, 95% CI: -0.7 to 28.5, P=0.063). Whites had an overall significant 3.1% AAPC (95% CI: 2.6 to 3.7, P< 0.001). There was no significant change in 1999-2005 (APC: -0.2%, 95% CI: -1.2 to 0.7, P=0.618), but significant increases were seen in 2005-2018 (APC: 3.5%, 95% CI: 3.1 to 3.8%, P< 0.001) and 2018-2020 (APC: 11.6%, 95% CI: 5.5 to 18.1, P=0.001). API had an overall significant 2.5% AAPC (95% CI: 1.2 to 3.8, P< 0.001); no significant increase seen in 1999-2013 (APC: 0.5%, 95% CI: -0.7 to 1.7%, P=0.409) but a significant increase in 2013-2020 was observed (APC: 6.6%, 95% CI: 3.1 to 10.3%, P=0.001). AI/AN had an overall significant 2.4% AAPC (95% CI: 1.0 to 3.8, P=0.001); non-significant decrease in 1999-2005 (APC: -1.7%, 95% CI: -3.8 to 0.6, P=0.129), significant increase in 2005-2018 (APC: 2.7%, 95% CI: 1.9 to 3.5%, P< 0.001) and a non-significant increase in 2018-2020 (APC: 13.4%, 95% CI: -0.7 to 29.4, P=0.062).
Discussion: From 1999-2020, mortality in ALD increased, with trends varying among races/ethnicities: AA displayed a non-significant overall trend, while Whites, API, and AI/AN showed significant increase with varied segments. ALD mortality remains a critical public health concern, with notable differences across demographics.

Figure: Figure 1: Ethnic and Racial Disparities in Alcoholic Liver Disease Related Mortality Rates
Disclosures:
Fariha Ilyas indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Stephanie Ibarra indicated no relevant financial relationships.
Pratik Patel indicated no relevant financial relationships.
Alexa Giammarino indicated no relevant financial relationships.
Sanjaya Satapathy indicated no relevant financial relationships.
Fariha Ilyas, MD1, Hassam Ali, MD1, Stephanie Ibarra, MD1, Pratik Patel, MD2, Alexa Giammarino, MD3, Sanjaya Satapathy, MD3. P0962 - Ethnic and Racial Disparities in Alcoholic Liver Disease Related Mortality: Data From CDC Wonder 1999-2020, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
