Sunday Poster Session
Category: IBD
P0685 - Real-World Clinical Effectiveness and Safety of Vedolizumab and Ustekinumab in Bio-Naïve Patients With Early Crohn’s Disease: Results from the EVOLVE Expansion Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Britt Christensen, MD
University of Melbourne and Royal Melbourne Hospital
Melbourne, Victoria, Australia
Presenting Author(s)
Award: Presidential Poster Award
Britt Christensen, MD1, Michael Scharl, MD2, Brian Bressler, MD, MS, FRCPC3, Zaeem Khan, MPH4, Yuliya Halchenko, MA5, Pravin Kamble, PhD6, Shashi Adsul, MD, MBA6, Zeinab Farhat, PhD6, Marc Ferrante, MD7
1University of Melbourne and Royal Melbourne Hospital, Melbourne, Victoria, Australia; 2University of Zurich, Zurich, Zurich, Switzerland; 3St. Paul’s Hospital, Vancouver, BC, Canada; 4PPD, part of Thermo Fisher Scientific, Montreal, PQ, Canada; 5PPD, Part of Thermo Fisher Scientific, Montreal, PQ, Canada; 6Takeda Pharmaceuticals, Cambridge, MA; 7University Hospitals Leuven, Leuven, Vlaams-Brabant, Belgium
Introduction: There is limited data comparing real-world clinical effectiveness and safety of vedolizumab (VDZ) and ustekinumab (UST) in patients (pts) with early Crohn’s Disease (CD, with a disease duration ≤2 years).
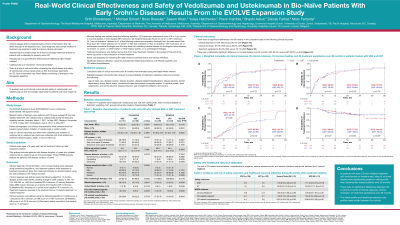
Methods: EVOLVE Expansion (NCT05056441) was a multicenter, observational, retrospective medical chart review study in biologic-naïve pts with CD (≥18 years old) who initiated VDZ or UST treatment in Australia, Belgium, or Switzerland from 2016 to 2021. This analysis looked at treatment outcomes in patients with early treatment (disease duration ≤2 years) who initiated VDZ or UST as first-line biologic. Data were collected from treatment initiation to chart abstraction, treatment discontinuation, death, or loss to follow-up. Cumulative rates of clinical response, remission, mucosal healing, and treatment persistence were estimated using the Kaplan Meier method over 12, 24 and 36 months. Serious adverse events (SAEs), serious infections (SIs), CD exacerbations, and CD-related hospitalization and surgeries were also evaluated. Baseline demographic and clinical characteristics across treatment groups were balanced using inverse probability weighting (IPW).
Results: There were 141 VDZ and 108 UST pts with early treatment. After IPW, both groups had similar baseline characteristics (Table 1). Over 36 months, cumulative rates were similar between VDZ- and UST-treated pts for clinical response (VDZ 80.8%, UST 79.0%; p=0.52) and clinical remission (VDZ 85.3%, UST 82.8%; p=0.52). Mucosal healing rates were significantly higher in VDZ- versus UST-treated pts (VDZ 92.5%, UST 87.0%, p=0.02). Treatment persistence (VDZ 64.6%, UST 76.7%; p=0.57) was not significantly different over 36 months. There were no significant differences in the risk of safety outcomes: SAEs (hazard ratio [HR]=1.23; CI 0.56-2.72; p=0.60), SIs (HR=6.57; CI 0.44-98.04; p=0.17), CD exacerbations (HR=1.07; CI 0.65-1.75; p=0.79), CD-related surgeries (HR=0.82; CI 0.38-1.76; p=0.61) or CD-related hospitalizations (HR=0.83; CI 0.35-1.95; p=0.67).
Discussion: In CD pts with early initiation of biologic treatment, rates of mucosal healing were significantly greater with VDZ vs UST. There were no significant differences between the VDZ and UST cohorts in clinical remission, clinical response, or treatment persistence. The probability of mucosal healing was significantly greater in pts treated with VDZ. The risk of CD-related hospitalization, surgeries, SAEs and SIs was similar between cohorts.
Disclosures:
Britt Christensen, MD1, Michael Scharl, MD2, Brian Bressler, MD, MS, FRCPC3, Zaeem Khan, MPH4, Yuliya Halchenko, MA5, Pravin Kamble, PhD6, Shashi Adsul, MD, MBA6, Zeinab Farhat, PhD6, Marc Ferrante, MD7. P0685 - Real-World Clinical Effectiveness and Safety of Vedolizumab and Ustekinumab in Bio-Naïve Patients With Early Crohn’s Disease: Results from the EVOLVE Expansion Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Britt Christensen, MD1, Michael Scharl, MD2, Brian Bressler, MD, MS, FRCPC3, Zaeem Khan, MPH4, Yuliya Halchenko, MA5, Pravin Kamble, PhD6, Shashi Adsul, MD, MBA6, Zeinab Farhat, PhD6, Marc Ferrante, MD7
1University of Melbourne and Royal Melbourne Hospital, Melbourne, Victoria, Australia; 2University of Zurich, Zurich, Zurich, Switzerland; 3St. Paul’s Hospital, Vancouver, BC, Canada; 4PPD, part of Thermo Fisher Scientific, Montreal, PQ, Canada; 5PPD, Part of Thermo Fisher Scientific, Montreal, PQ, Canada; 6Takeda Pharmaceuticals, Cambridge, MA; 7University Hospitals Leuven, Leuven, Vlaams-Brabant, Belgium
Introduction: There is limited data comparing real-world clinical effectiveness and safety of vedolizumab (VDZ) and ustekinumab (UST) in patients (pts) with early Crohn’s Disease (CD, with a disease duration ≤2 years).
Methods: EVOLVE Expansion (NCT05056441) was a multicenter, observational, retrospective medical chart review study in biologic-naïve pts with CD (≥18 years old) who initiated VDZ or UST treatment in Australia, Belgium, or Switzerland from 2016 to 2021. This analysis looked at treatment outcomes in patients with early treatment (disease duration ≤2 years) who initiated VDZ or UST as first-line biologic. Data were collected from treatment initiation to chart abstraction, treatment discontinuation, death, or loss to follow-up. Cumulative rates of clinical response, remission, mucosal healing, and treatment persistence were estimated using the Kaplan Meier method over 12, 24 and 36 months. Serious adverse events (SAEs), serious infections (SIs), CD exacerbations, and CD-related hospitalization and surgeries were also evaluated. Baseline demographic and clinical characteristics across treatment groups were balanced using inverse probability weighting (IPW).
Results: There were 141 VDZ and 108 UST pts with early treatment. After IPW, both groups had similar baseline characteristics (Table 1). Over 36 months, cumulative rates were similar between VDZ- and UST-treated pts for clinical response (VDZ 80.8%, UST 79.0%; p=0.52) and clinical remission (VDZ 85.3%, UST 82.8%; p=0.52). Mucosal healing rates were significantly higher in VDZ- versus UST-treated pts (VDZ 92.5%, UST 87.0%, p=0.02). Treatment persistence (VDZ 64.6%, UST 76.7%; p=0.57) was not significantly different over 36 months. There were no significant differences in the risk of safety outcomes: SAEs (hazard ratio [HR]=1.23; CI 0.56-2.72; p=0.60), SIs (HR=6.57; CI 0.44-98.04; p=0.17), CD exacerbations (HR=1.07; CI 0.65-1.75; p=0.79), CD-related surgeries (HR=0.82; CI 0.38-1.76; p=0.61) or CD-related hospitalizations (HR=0.83; CI 0.35-1.95; p=0.67).
Discussion: In CD pts with early initiation of biologic treatment, rates of mucosal healing were significantly greater with VDZ vs UST. There were no significant differences between the VDZ and UST cohorts in clinical remission, clinical response, or treatment persistence. The probability of mucosal healing was significantly greater in pts treated with VDZ. The risk of CD-related hospitalization, surgeries, SAEs and SIs was similar between cohorts.
Table: Table: Baseline Characteristics
Disclosures:
Britt Christensen: AbbVie – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. BMS – Advisory Committee/Board Member, Speakers Bureau. Celltrion – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Falk – Advisory Committee/Board Member, Speakers Bureau. Ferring – Advisory Committee/Board Member, Speakers Bureau. Fresenius Kabi – Advisory Committee/Board Member, Speakers Bureau. Gilead – Advisory Committee/Board Member, Speakers Bureau. Janssen – Grant/Research Support. Janssen-Cilag – Advisory Committee/Board Member, Speakers Bureau. MSD – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Sandoz – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau.
Michael Scharl: AbbVie – Grant/Research Support. Axalbion – Grant/Research Support. Basilea Pharmaceuticals – Grant/Research Support. Calypso Biotech – Grant/Research Support. Celltrion – Consultant. Falk Pharma – Speakers Bureau. Fresenius – Consultant. Gilead – Consultant, Grant/Research Support. Herbodee – Grant/Research Support. NodThera – Grant/Research Support. PharmaBiome – Grant/Research Support, Stock Options. Recolony – Stock Options. Roche – Grant/Research Support. Takeda – Consultant, Grant/Research Support. Topadur – Consultant. Vifor – Grant/Research Support, Speakers Bureau. Zealand Pharma – Grant/Research Support.
Brian Bressler: AbbVie – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Alimentiv – Advisory Committee/Board Member. Allergan – Advisory Committee/Board Member. Alvine – Grant/Research Support. Amgen – Advisory Committee/Board Member, Grant/Research Support. AMT – Advisory Committee/Board Member. Bausch Health – Advisory Committee/Board Member. Boehringer Ingelheim – Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Celgene – Advisory Committee/Board Member, Grant/Research Support. Ferring – Advisory Committee/Board Member, Speakers Bureau. Fresenius Kabi – Advisory Committee/Board Member. Genentech – Advisory Committee/Board Member, Grant/Research Support. Gilead – Advisory Committee/Board Member. GlaxoSmithKline – Grant/Research Support. Iterative Scopes – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Merck – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Microbiome Insights – Advisory Committee/Board Member. Mylan – Advisory Committee/Board Member. Novartis – Advisory Committee/Board Member, Speakers Bureau. Pendopharm – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Speakers Bureau. Protagonist – Advisory Committee/Board Member. Qu Biologic – Grant/Research Support, Stock Options. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Zaeem Khan: PPD, part of Thermo Fisher Scientific – Employee.
Yuliya Halchenko: PPD, Part of Thermo Fisher Scientific – Employee.
Pravin Kamble: Takeda – Employee, Stock Options.
Shashi Adsul: Takeda – Employee, Stock Options.
Zeinab Farhat: Takeda – Employee, Stock Options.
Marc Ferrante: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. AgomAb Therapeutics – Consultant. Amgen – Grant/Research Support, Speakers Bureau. Biogen – Grant/Research Support, Speakers Bureau. Boehringer Ingelheim – Consultant, Speakers Bureau. Celgene – Consultant. Celltrion – Consultant. EG – Grant/Research Support. Eli Lily – Consultant. Falk – Speakers Bureau. Ferring – Speakers Bureau. Janssen – Grant/Research Support. Janssen-Cilag – Consultant, Speakers Bureau. Lamepro – Speakers Bureau. Medtronic – Consultant. MSD – Consultant, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Regeneron – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant, Speakers Bureau. Takeda – Consultant, Grant/Research Support, Speakers Bureau. Thermo Fisher – Consultant. Truvion Healthcare – Speakers Bureau. Viatris – Grant/Research Support, Speakers Bureau.
Britt Christensen, MD1, Michael Scharl, MD2, Brian Bressler, MD, MS, FRCPC3, Zaeem Khan, MPH4, Yuliya Halchenko, MA5, Pravin Kamble, PhD6, Shashi Adsul, MD, MBA6, Zeinab Farhat, PhD6, Marc Ferrante, MD7. P0685 - Real-World Clinical Effectiveness and Safety of Vedolizumab and Ustekinumab in Bio-Naïve Patients With Early Crohn’s Disease: Results from the EVOLVE Expansion Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

