Sunday Poster Session
Category: Esophagus
P0500 - Poor Consumption: A Case of Gastrointestinal Tuberculosis Mimicking Malignancy in an Immunocompromised Patient
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Shae Patel, DO
Loma Linda University Health
Placentia, CA
Presenting Author(s)
Award: Presidential Poster Award
Shae Patel, DO1, Devika Gandhi, MD2, Andrei Tong, BA2, Ansel Nam, MD3, Nour Parsa, MD4
1Loma Linda University Health, Placentia, CA; 2Loma Linda University, Loma Linda, CA; 3Loma Linda University Health Education Consortium, Loma Linda, CA; 4Loma Linda University Health, Loma Linda, CA
Introduction: Mycobacterium tuberculosis (TB) is a leading infectious cause of morbidity and mortality globally. In 2021, an estimated 10.6 million people contracted TB with 1.6 million people dying from TB worldwide. Esophageal and gastric manifestations of TB are rare, but can occur in the presence or absence of pulmonary tuberculosis. Herein, we present a case of disseminated tuberculosis with primary esophageal and gastric manifestations mimicking malignancy in an immunocompromised patient.
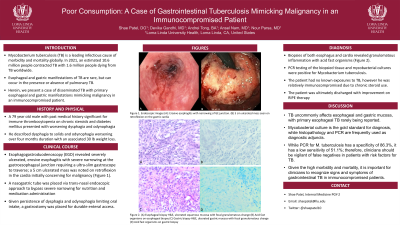
Case Description/Methods: A 79 year old male with past history significant for immune thrombocytopenia on chronic steroids and diabetes mellitus presented for worsening dysphagia and odynophagia. He described dysphagia to solids and odynophagia worsening over four months duration with an associated 30 lbs weight loss. Esophagogastroduodenoscopy (EGD) revealed severely ulcerated, erosive esophagitis with severe narrowing at gastroesophageal junction requiring ultra-slim gastroscope to traverse and 5 cm ulcerated mass noted on retroflexion in the cardia initially concerning for malignancy. A nasogastric tube was placed via transnasal endoscopic approach to bypass severe narrowing for nutrition and medication administration. Biopsies of both esophagus and cardia revealed granulomatous inflammation with acid fast organisms. PCR testing of the biopsied tissue and ultimately mycobacterial cultures were positive for M. tuberculosis. The patient had no known exposures to tuberculosis, however he was relatively immunocompromised due to chronic steroid use. The patient was started on rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) for treatment of disseminated tuberculosis. Given persistence of dysphagia and odynophagia limiting oral intake, a gastrostomy tube was placed for durable enteral access. The patient was ultimately discharged with improvement on RIPE therapy.
Discussion: Tuberculosis uncommonly affects esophageal and gastric mucosa, with primary esophageal TB rarely being reported. Mycobacterial culture is the gold standard for diagnosis, histopathology and PCR are frequently used as diagnostic adjuncts. While PCR for M. tuberculosis has a specificity of 86.3%, it has a low sensitivity of 51.1% thus clinicians should be vigilant of false negatives in patients with risk factors for tuberculosis. Given the high morbidity and mortality, it is important that clinicians are able to recognize signs and symptoms of gastrointestinal tuberculosis in immunocompromised patients.

Disclosures:
Shae Patel, DO1, Devika Gandhi, MD2, Andrei Tong, BA2, Ansel Nam, MD3, Nour Parsa, MD4. P0500 - Poor Consumption: A Case of Gastrointestinal Tuberculosis Mimicking Malignancy in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Shae Patel, DO1, Devika Gandhi, MD2, Andrei Tong, BA2, Ansel Nam, MD3, Nour Parsa, MD4
1Loma Linda University Health, Placentia, CA; 2Loma Linda University, Loma Linda, CA; 3Loma Linda University Health Education Consortium, Loma Linda, CA; 4Loma Linda University Health, Loma Linda, CA
Introduction: Mycobacterium tuberculosis (TB) is a leading infectious cause of morbidity and mortality globally. In 2021, an estimated 10.6 million people contracted TB with 1.6 million people dying from TB worldwide. Esophageal and gastric manifestations of TB are rare, but can occur in the presence or absence of pulmonary tuberculosis. Herein, we present a case of disseminated tuberculosis with primary esophageal and gastric manifestations mimicking malignancy in an immunocompromised patient.
Case Description/Methods: A 79 year old male with past history significant for immune thrombocytopenia on chronic steroids and diabetes mellitus presented for worsening dysphagia and odynophagia. He described dysphagia to solids and odynophagia worsening over four months duration with an associated 30 lbs weight loss. Esophagogastroduodenoscopy (EGD) revealed severely ulcerated, erosive esophagitis with severe narrowing at gastroesophageal junction requiring ultra-slim gastroscope to traverse and 5 cm ulcerated mass noted on retroflexion in the cardia initially concerning for malignancy. A nasogastric tube was placed via transnasal endoscopic approach to bypass severe narrowing for nutrition and medication administration. Biopsies of both esophagus and cardia revealed granulomatous inflammation with acid fast organisms. PCR testing of the biopsied tissue and ultimately mycobacterial cultures were positive for M. tuberculosis. The patient had no known exposures to tuberculosis, however he was relatively immunocompromised due to chronic steroid use. The patient was started on rifampin, isoniazid, pyrazinamide, and ethambutol (RIPE) for treatment of disseminated tuberculosis. Given persistence of dysphagia and odynophagia limiting oral intake, a gastrostomy tube was placed for durable enteral access. The patient was ultimately discharged with improvement on RIPE therapy.
Discussion: Tuberculosis uncommonly affects esophageal and gastric mucosa, with primary esophageal TB rarely being reported. Mycobacterial culture is the gold standard for diagnosis, histopathology and PCR are frequently used as diagnostic adjuncts. While PCR for M. tuberculosis has a specificity of 86.3%, it has a low sensitivity of 51.1% thus clinicians should be vigilant of false negatives in patients with risk factors for tuberculosis. Given the high morbidity and mortality, it is important that clinicians are able to recognize signs and symptoms of gastrointestinal tuberculosis in immunocompromised patients.

Figure: Figure 1: Endoscopic images (A): Erosive esophagitis with narrowing of GE junction. (B) 5cm ulcerated mass seen on retroflexion on the gastric cardia
Disclosures:
Shae Patel indicated no relevant financial relationships.
Devika Gandhi indicated no relevant financial relationships.
Andrei Tong indicated no relevant financial relationships.
Ansel Nam indicated no relevant financial relationships.
Nour Parsa indicated no relevant financial relationships.
Shae Patel, DO1, Devika Gandhi, MD2, Andrei Tong, BA2, Ansel Nam, MD3, Nour Parsa, MD4. P0500 - Poor Consumption: A Case of Gastrointestinal Tuberculosis Mimicking Malignancy in an Immunocompromised Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

