Sunday Poster Session
Category: Colon
P0268 - Where Sunscreen Can’t Help: Rectal Malignant Melanoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Sindhura Kolli, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sindhura Kolli, MD1, Mel Ona, MD, MS, MPH, MA2, Janelle Otsuji, MD2, Anthony Michaud, MD3, Melvin Palalay, MD4
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Pali Momi Medical Center, Aiea, HI; 3Queen's Medical Center, Honolulu, HI; 4Hawaii Cancer Care, Honolulu, HI
Introduction: Rectal malignant melanoma (MM) is vastly different from cutaneous MM. These differences are vital for recognition and a timely diagnosis. Here we present a rare case of rectal MM with a surprising response to treatments most have written off as palliative.
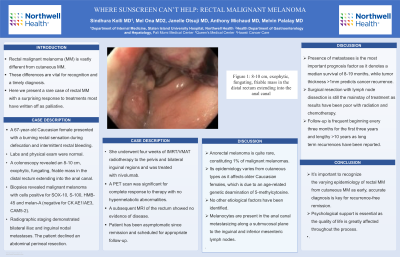
Case Description/Methods: A 67-year-old Caucasian female presented with a burning rectal sensation during defecation and intermittent rectal bleeding. Labs and physical exam were normal. A colonoscopy revealed an 8-10 cm, exophytic, fungating, friable mass in the distal rectum extending into the anal canal. Biopsies revealed malignant melanoma with cells positive for SOX-10, S-100, HMB-45 and melan-A (negative for CK AE1/AE3, CAM5-2). Radiographic staging demonstrated bilateral iliac and inguinal nodal metastases. The patient declined an abdominal perineal resection. She underwent four weeks of IMRT/VMAT radiotherapy to the pelvis and bilateral inguinal regions and was treated with nivolumab. A PET scan was significant for complete response to therapy with no hypermetabolic abnormalities. A subsequent MRI of the rectum showed no evidence of disease. Patient has been asymptomatic since remission and scheduled for appropriate follow-up.
Discussion: Anorectal melanoma is quite rare, constituting 1% of malignant melanomas. Its epidemiology varies from cutaneous types as it affects older Caucasian females, which is due to an age-related genetic deamination of 5-methylcytosine. No other etiological factors have been identified. Melanocytes are present in the anal canal metastasizing along a submucosal plane to the inguinal and inferior mesenteric lymph nodes. Presence of metastases is the most important prognosis factor as it denotes a median survival of 8-19 months, while tumor thickness >1mm predicts cancer recurrence. Surgical resection with lymph node dissection is still the mainstay of treatment as results have been poor with radiation and chemotherapy. Follow up is frequent starting with every three months for the first three years and lengthy >10 years as long term recurrences have been reported. It’s important to recognize the varying epidemiology of rectal MM from cutaneous MM as early, accurate diagnosis is key for recurrence-free remission. Psychological support is essential as the quality of life is greatly affected throughout the process.

Disclosures:
Sindhura Kolli, MD1, Mel Ona, MD, MS, MPH, MA2, Janelle Otsuji, MD2, Anthony Michaud, MD3, Melvin Palalay, MD4. P0268 - Where Sunscreen Can’t Help: Rectal Malignant Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Pali Momi Medical Center, Aiea, HI; 3Queen's Medical Center, Honolulu, HI; 4Hawaii Cancer Care, Honolulu, HI
Introduction: Rectal malignant melanoma (MM) is vastly different from cutaneous MM. These differences are vital for recognition and a timely diagnosis. Here we present a rare case of rectal MM with a surprising response to treatments most have written off as palliative.
Case Description/Methods: A 67-year-old Caucasian female presented with a burning rectal sensation during defecation and intermittent rectal bleeding. Labs and physical exam were normal. A colonoscopy revealed an 8-10 cm, exophytic, fungating, friable mass in the distal rectum extending into the anal canal. Biopsies revealed malignant melanoma with cells positive for SOX-10, S-100, HMB-45 and melan-A (negative for CK AE1/AE3, CAM5-2). Radiographic staging demonstrated bilateral iliac and inguinal nodal metastases. The patient declined an abdominal perineal resection. She underwent four weeks of IMRT/VMAT radiotherapy to the pelvis and bilateral inguinal regions and was treated with nivolumab. A PET scan was significant for complete response to therapy with no hypermetabolic abnormalities. A subsequent MRI of the rectum showed no evidence of disease. Patient has been asymptomatic since remission and scheduled for appropriate follow-up.
Discussion: Anorectal melanoma is quite rare, constituting 1% of malignant melanomas. Its epidemiology varies from cutaneous types as it affects older Caucasian females, which is due to an age-related genetic deamination of 5-methylcytosine. No other etiological factors have been identified. Melanocytes are present in the anal canal metastasizing along a submucosal plane to the inguinal and inferior mesenteric lymph nodes. Presence of metastases is the most important prognosis factor as it denotes a median survival of 8-19 months, while tumor thickness >1mm predicts cancer recurrence. Surgical resection with lymph node dissection is still the mainstay of treatment as results have been poor with radiation and chemotherapy. Follow up is frequent starting with every three months for the first three years and lengthy >10 years as long term recurrences have been reported. It’s important to recognize the varying epidemiology of rectal MM from cutaneous MM as early, accurate diagnosis is key for recurrence-free remission. Psychological support is essential as the quality of life is greatly affected throughout the process.

Figure: Figure 1: 8-10 cm, exophytic, fungating, friable mass in the distal rectum extending into the anal canal
Disclosures:
Sindhura Kolli indicated no relevant financial relationships.
Mel Ona indicated no relevant financial relationships.
Janelle Otsuji indicated no relevant financial relationships.
Anthony Michaud indicated no relevant financial relationships.
Melvin Palalay indicated no relevant financial relationships.
Sindhura Kolli, MD1, Mel Ona, MD, MS, MPH, MA2, Janelle Otsuji, MD2, Anthony Michaud, MD3, Melvin Palalay, MD4. P0268 - Where Sunscreen Can’t Help: Rectal Malignant Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
