Sunday Poster Session
Category: Colon
P0269 - Definitely Not Crohn’s: Epstein Barr Virus Positive Mucocutaneous Lymphoproliferative Intestinal Ulcer Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Sindhura Kolli, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sindhura Kolli, MD1, Shivantha Amarnath, MD2, Mark Grief, MD3, Owen Chan, MD4, Mel Ona, MD, MS, MPH, MA3
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Staten Island, NY; 3Pali Momi Medical Center, Aiea, HI; 4Pali Momi Medical Center, Aeia, HI
Introduction: Epstein Barr virus (EBV) positive mucocutaneous ulcer disease is a rare lymphoproliferative process that rarely occurs in the colon. It's not associated with detectable levels of serum EBV, so is often misdiagnosed as Crohn’s disease. We present a tubular adenoma superimposed on a right-sided colonic ulcer positive for EBV in an immunocompetent patient.
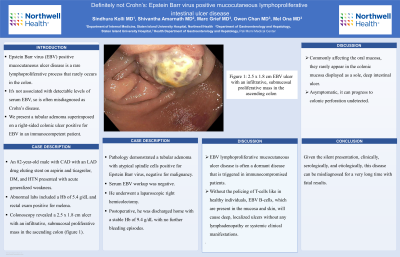
Case Description/Methods: An 82-year-old male with CAD with an LAD drug eluting stent on aspirin and ticagrelor, DM, and HTN presented with acute generalized weakness. Abnormal labs included a Hb of 5.4 g/dL and rectal exam positive for melena. Colonoscopy revealed a 2.5 x 1.8 cm ulcer with an infiltrative, submucosal proliferative mass in the ascending colon (figure 1). Pathology demonstrated a tubular adenoma with atypical spindle cells positive for Epstein Barr virus, negative for malignancy. Serum EBV workup was negative. He underwent a laparoscopic right hemicolectomy. Postoperative, he was discharged home with a stable Hb of 9.4 g/dL with no further bleeding episodes.
Discussion: EBV lymphoproliferative mucocutaneous ulcer disease is often a dormant disease that is triggered in immunocompromised patients. Without the policing of T-cells like in healthy individuals, EBV B-cells, which are present in the mucosa and skin, will cause deep, localized ulcers without any lymphadenopathy or systemic clinical manifestations. Commonly affecting the oral mucosa, they rarely appear in the colonic mucosa displayed as a sole, deep intestinal ulcer. Asymptomatic, it can progress to colonic perforation undetected. While our patient did not have immunocompromising risk factors, we suspect age-associated immunosenescence triggered an active disease, which can have a relapsing/remitting course before spontaneous improvement. Persistent or symptomatic courses have benefited from the use of rituximab, a CD-20 B-cell antibody or localized resection. Given the silent presentation, clinically, serologically, and etiologically, this disease can be misdiagnosed for a very long time with fatal results.
Disclosures:
Sindhura Kolli, MD1, Shivantha Amarnath, MD2, Mark Grief, MD3, Owen Chan, MD4, Mel Ona, MD, MS, MPH, MA3. P0269 - Definitely Not Crohn’s: Epstein Barr Virus Positive Mucocutaneous Lymphoproliferative Intestinal Ulcer Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Staten Island, NY; 3Pali Momi Medical Center, Aiea, HI; 4Pali Momi Medical Center, Aeia, HI
Introduction: Epstein Barr virus (EBV) positive mucocutaneous ulcer disease is a rare lymphoproliferative process that rarely occurs in the colon. It's not associated with detectable levels of serum EBV, so is often misdiagnosed as Crohn’s disease. We present a tubular adenoma superimposed on a right-sided colonic ulcer positive for EBV in an immunocompetent patient.
Case Description/Methods: An 82-year-old male with CAD with an LAD drug eluting stent on aspirin and ticagrelor, DM, and HTN presented with acute generalized weakness. Abnormal labs included a Hb of 5.4 g/dL and rectal exam positive for melena. Colonoscopy revealed a 2.5 x 1.8 cm ulcer with an infiltrative, submucosal proliferative mass in the ascending colon (figure 1). Pathology demonstrated a tubular adenoma with atypical spindle cells positive for Epstein Barr virus, negative for malignancy. Serum EBV workup was negative. He underwent a laparoscopic right hemicolectomy. Postoperative, he was discharged home with a stable Hb of 9.4 g/dL with no further bleeding episodes.
Discussion: EBV lymphoproliferative mucocutaneous ulcer disease is often a dormant disease that is triggered in immunocompromised patients. Without the policing of T-cells like in healthy individuals, EBV B-cells, which are present in the mucosa and skin, will cause deep, localized ulcers without any lymphadenopathy or systemic clinical manifestations. Commonly affecting the oral mucosa, they rarely appear in the colonic mucosa displayed as a sole, deep intestinal ulcer. Asymptomatic, it can progress to colonic perforation undetected. While our patient did not have immunocompromising risk factors, we suspect age-associated immunosenescence triggered an active disease, which can have a relapsing/remitting course before spontaneous improvement. Persistent or symptomatic courses have benefited from the use of rituximab, a CD-20 B-cell antibody or localized resection. Given the silent presentation, clinically, serologically, and etiologically, this disease can be misdiagnosed for a very long time with fatal results.
Disclosures:
Sindhura Kolli indicated no relevant financial relationships.
Shivantha Amarnath indicated no relevant financial relationships.
Mark Grief indicated no relevant financial relationships.
Owen Chan indicated no relevant financial relationships.
Mel Ona indicated no relevant financial relationships.
Sindhura Kolli, MD1, Shivantha Amarnath, MD2, Mark Grief, MD3, Owen Chan, MD4, Mel Ona, MD, MS, MPH, MA3. P0269 - Definitely Not Crohn’s: Epstein Barr Virus Positive Mucocutaneous Lymphoproliferative Intestinal Ulcer Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
