Sunday Poster Session
Category: Colon
P0277 - TB or Not TB?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Patricia Miguez Arosemena, MD
Mount Sinai West and Morningside
New York, NY
Presenting Author(s)
Jenny Dave, MD, MS1, Patricia Miguez Arosemena, MD1, Priya Simoes, MD2
1Mount Sinai West and Morningside, New York, NY; 2Mount Sinai Morningside and West, New York, NY
Introduction: Gastrointestinal (GI) tuberculosis (TB) accounts for 1 to 3% of all TB cases worldwide (Chakinala, 2022). If left undiagnosed and untreated, it can cause significant morbidity with up to a 60% mortality (Chan, 2015). Most prevalent in Africa and Asia, western countries are seeing a rise in cases largely due to immunocompromising disease, biologic use and migration. However given the low rate of cases in the U.S. and non-specific symptoms, GI TB is not always on the clinicians differential for patients with common risk factors which may lead to a delay in diagnosis and treatment. We present a case of ileal tuberculosis in an elderly female.
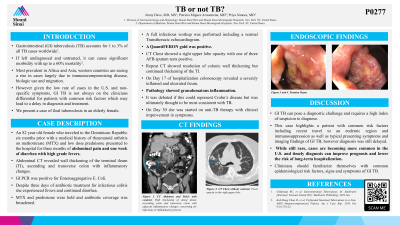
Case Description/Methods: An 82 year old female who traveled to the Dominican Republic six months prior with a medical history of rheumatoid arthritis on methotrexate (MTX) and low dose prednisone presented to the hospital for three months of abdominal pain and one week of diarrhea with high grade fevers. Abdominal CT revealed wall thickening of the terminal ileum (TI), ascending and transverse colon with inflammatory changes. GI PCR was positive for Enteroaggregative E. Coli. Despite three days of antibiotic treatment for infectious colitis she experienced fevers and continued diarrhea. MTX and prednisone were held and antibiotic coverage was broadened. A full infectious workup was performed including a normal Transthoracic echocardiogram. A QuantiFERON gold was positive. CT Chest showed a right upper lobe opacity with one of three AFB sputum tests positive. Repeat CT showed resolution of colonic wall thickening but continued thickening of the TI. On Day 17 of hospitalization colonoscopy revealed a severely inflamed and ulcerated ileum. Pathology showed granulomatous inflammation. It was debated if this could represent Crohn’s disease but was ultimately thought to be most consistent with TB. On Day 30 she was started on anti-TB therapy with clinical improvement in symptoms.
Discussion: GI TB can pose a diagnostic challenge and requires a high index of suspicion to diagnose. This case highlights a patient with common risk factors including recent travel to an endemic region and immunosuppression as well as typical presenting symptoms and imaging findings of GI TB, however diagnosis was still delayed. While still rare, cases are becoming more common in the U.S. and timely diagnosis can improve prognosis and lower the risk of long-term hospitalization. Clinicians should familiarize themselves with common epidemiological risk factors, signs and symptoms of GI TB.
Disclosures:
Jenny Dave, MD, MS1, Patricia Miguez Arosemena, MD1, Priya Simoes, MD2. P0277 - TB or Not TB?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai West and Morningside, New York, NY; 2Mount Sinai Morningside and West, New York, NY
Introduction: Gastrointestinal (GI) tuberculosis (TB) accounts for 1 to 3% of all TB cases worldwide (Chakinala, 2022). If left undiagnosed and untreated, it can cause significant morbidity with up to a 60% mortality (Chan, 2015). Most prevalent in Africa and Asia, western countries are seeing a rise in cases largely due to immunocompromising disease, biologic use and migration. However given the low rate of cases in the U.S. and non-specific symptoms, GI TB is not always on the clinicians differential for patients with common risk factors which may lead to a delay in diagnosis and treatment. We present a case of ileal tuberculosis in an elderly female.
Case Description/Methods: An 82 year old female who traveled to the Dominican Republic six months prior with a medical history of rheumatoid arthritis on methotrexate (MTX) and low dose prednisone presented to the hospital for three months of abdominal pain and one week of diarrhea with high grade fevers. Abdominal CT revealed wall thickening of the terminal ileum (TI), ascending and transverse colon with inflammatory changes. GI PCR was positive for Enteroaggregative E. Coli. Despite three days of antibiotic treatment for infectious colitis she experienced fevers and continued diarrhea. MTX and prednisone were held and antibiotic coverage was broadened. A full infectious workup was performed including a normal Transthoracic echocardiogram. A QuantiFERON gold was positive. CT Chest showed a right upper lobe opacity with one of three AFB sputum tests positive. Repeat CT showed resolution of colonic wall thickening but continued thickening of the TI. On Day 17 of hospitalization colonoscopy revealed a severely inflamed and ulcerated ileum. Pathology showed granulomatous inflammation. It was debated if this could represent Crohn’s disease but was ultimately thought to be most consistent with TB. On Day 30 she was started on anti-TB therapy with clinical improvement in symptoms.
Discussion: GI TB can pose a diagnostic challenge and requires a high index of suspicion to diagnose. This case highlights a patient with common risk factors including recent travel to an endemic region and immunosuppression as well as typical presenting symptoms and imaging findings of GI TB, however diagnosis was still delayed. While still rare, cases are becoming more common in the U.S. and timely diagnosis can improve prognosis and lower the risk of long-term hospitalization. Clinicians should familiarize themselves with common epidemiological risk factors, signs and symptoms of GI TB.
Disclosures:
Jenny Dave indicated no relevant financial relationships.
Patricia Miguez Arosemena indicated no relevant financial relationships.
Priya Simoes indicated no relevant financial relationships.
Jenny Dave, MD, MS1, Patricia Miguez Arosemena, MD1, Priya Simoes, MD2. P0277 - TB or Not TB?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
