Sunday Poster Session
Category: Biliary/Pancreas
P0059 - Hepatopulmonary Fistula With Bilioptysis as a Complication of Radical Hepatobiliary Reconstruction
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Wesley A. Robertson, MD, MPH, MPA
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Award: Presidential Poster Award
Wesley A.. Robertson, MD, MPH, MPA1, Pierce Lewien, MD2, Christopher Alvarez, MD3, Teodor Pitea, MD3, Nilda Franco, MD3
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona Phoenix, Phoenix, AZ; 3Banner University Medical Center, Phoenix, AZ
Introduction: Bronchopulmonary fistula is a rare clinical finding with high morbidity. Advanced hepatobiliary surgical techniques are being increasingly utilized with significant increase in iatrogenic fistulas following liver resection or ablation therapy. Patients typically present with a wide range of symptoms, including fever, abdominal pain, jaundice, bilious sputum. Untreated fistula can quickly lead to sepsis progressing to fulminant acute respiratory distress syndrome. Here we describe a patient who presented with bright yellow sputum production due to hepatopulmonary fistula.
Case Description/Methods: A 40-year-old woman with history of metastatic right renal spindle cell sarcoma with hepatobiliary involvement underwent partial hepatectomy and extensive diaphragmatic resection with IVC reconstruction at outside hospital. She was discharged on immunotherapy and subsequently developed a productive cough. Evaluation at that time revealed liver abscess. Hepatic drain was placed and patient was discharged on antibiotics.
Patient presented to our institution with unresolved cough consisting of copious bright yellow sputum. CT Angio Chest and Abdomen/Pelvis demonstrated right middle and lower lobe consolidations, and complex fluid collection within liver. Bronchoscopy revealed bilious fluid concerning for hepatopulmonary fistula. Hepatobiliary surgery was consulted, deferring surgery given high risk. ERCP noted biliary papillary stenosis with common bile duct dilation. Biliary sphincterotomy was performed with multiple stents placed to pancreatic, common bile, and right hepatic duct to allow for healing of broncho-biliary fistula. Bilious sputum significantly improved and patient was discharged with repeat ERCP planned outpatient.
Discussion: Bronchopulmonary fistula is a rare surgical complication, and diagnosis is typically delayed as bilious fluid is not routinely assessed in sputum sampling. Presence of bile in sputum or pleural effusion is pathognomonic. MRI, MRCP, or HIDA scan can assist in establishing diagnosis. Management revolves around lowering biliary pressure through ERCP with stent placement and/or thoracostomy tube placement. Spontaneous closure happens in up to 60% of posttraumatic cases, otherwise surgical exploration via thoracotomy may be considered.
Clinicians should be aware of this rare complication in any patient who presents with recurrent pneumonia and fluid collection with copious yellow sputum after surgical intervention with diaphragmatic involvement.

Disclosures:
Wesley A.. Robertson, MD, MPH, MPA1, Pierce Lewien, MD2, Christopher Alvarez, MD3, Teodor Pitea, MD3, Nilda Franco, MD3. P0059 - Hepatopulmonary Fistula With Bilioptysis as a Complication of Radical Hepatobiliary Reconstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Wesley A.. Robertson, MD, MPH, MPA1, Pierce Lewien, MD2, Christopher Alvarez, MD3, Teodor Pitea, MD3, Nilda Franco, MD3
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona Phoenix, Phoenix, AZ; 3Banner University Medical Center, Phoenix, AZ
Introduction: Bronchopulmonary fistula is a rare clinical finding with high morbidity. Advanced hepatobiliary surgical techniques are being increasingly utilized with significant increase in iatrogenic fistulas following liver resection or ablation therapy. Patients typically present with a wide range of symptoms, including fever, abdominal pain, jaundice, bilious sputum. Untreated fistula can quickly lead to sepsis progressing to fulminant acute respiratory distress syndrome. Here we describe a patient who presented with bright yellow sputum production due to hepatopulmonary fistula.
Case Description/Methods: A 40-year-old woman with history of metastatic right renal spindle cell sarcoma with hepatobiliary involvement underwent partial hepatectomy and extensive diaphragmatic resection with IVC reconstruction at outside hospital. She was discharged on immunotherapy and subsequently developed a productive cough. Evaluation at that time revealed liver abscess. Hepatic drain was placed and patient was discharged on antibiotics.
Patient presented to our institution with unresolved cough consisting of copious bright yellow sputum. CT Angio Chest and Abdomen/Pelvis demonstrated right middle and lower lobe consolidations, and complex fluid collection within liver. Bronchoscopy revealed bilious fluid concerning for hepatopulmonary fistula. Hepatobiliary surgery was consulted, deferring surgery given high risk. ERCP noted biliary papillary stenosis with common bile duct dilation. Biliary sphincterotomy was performed with multiple stents placed to pancreatic, common bile, and right hepatic duct to allow for healing of broncho-biliary fistula. Bilious sputum significantly improved and patient was discharged with repeat ERCP planned outpatient.
Discussion: Bronchopulmonary fistula is a rare surgical complication, and diagnosis is typically delayed as bilious fluid is not routinely assessed in sputum sampling. Presence of bile in sputum or pleural effusion is pathognomonic. MRI, MRCP, or HIDA scan can assist in establishing diagnosis. Management revolves around lowering biliary pressure through ERCP with stent placement and/or thoracostomy tube placement. Spontaneous closure happens in up to 60% of posttraumatic cases, otherwise surgical exploration via thoracotomy may be considered.
Clinicians should be aware of this rare complication in any patient who presents with recurrent pneumonia and fluid collection with copious yellow sputum after surgical intervention with diaphragmatic involvement.

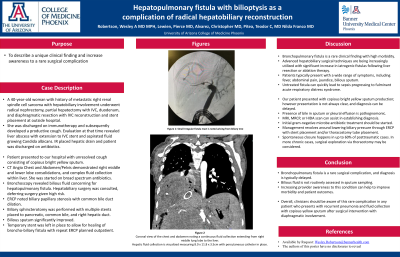
Figure: Figure 1a: Coronal view of the chest and abdomen noting a continuous fluid collection extending from right middlelung lobe to the liver. Hepatic fluid collection is visualized measuring 8.0 x 11.8 x 3.5cm withpercutaneous catheter in place.
Figure 1b: Small Irregular fistula tract is noted arising from biliary tree
Figure 1b: Small Irregular fistula tract is noted arising from biliary tree
Disclosures:
Wesley Robertson indicated no relevant financial relationships.
Pierce Lewien indicated no relevant financial relationships.
Christopher Alvarez indicated no relevant financial relationships.
Teodor Pitea indicated no relevant financial relationships.
Nilda Franco indicated no relevant financial relationships.
Wesley A.. Robertson, MD, MPH, MPA1, Pierce Lewien, MD2, Christopher Alvarez, MD3, Teodor Pitea, MD3, Nilda Franco, MD3. P0059 - Hepatopulmonary Fistula With Bilioptysis as a Complication of Radical Hepatobiliary Reconstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


