Sunday Poster Session
Category: Biliary/Pancreas
P0062 - Pancreatic Plasmacytoma Presenting as Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- RR
Rehan Razzaq, DO
Virginia Commonwealth University
Richmond, VA
Presenting Author(s)
Rehan Razzaq, DO1, Yasra Badi, MD2, Mahum Nadeem, MBBS3, Asiya Tafader, MBBS3, Joseph S.. Spataro, MD4
1Virginia Commonwealth University, Richmond, VA; 2HCA MountainView Hospital, Arlington, VA; 3Virginia Commonwealth University, Henrico, VA; 4Hunter Holmes Mcguire VA, Richmond, VA
Introduction: Extramedullary solitary plasmacytomas are an uncommon manifestation of plasma cell disorders. It is associated with a poor prognosis with a median survival rate of less than six months. Although rare to involve the digestive tract, the liver is the most common site, with pancreatic involvement demonstrating a 2.3% incidence rate. We report a case of pancreatic plasmacytoma in a patient with multiple myeloma (MM) presenting with painless obstructive jaundice.
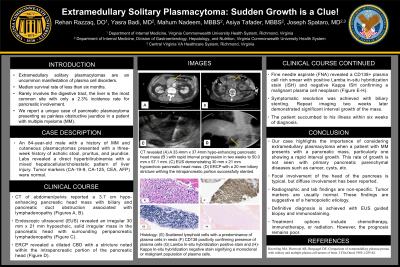
Case Description/Methods: An 84-year-old male with a history of MM and cutaneous plasmacytomas presented with a three-week onset of acholic stool, pruritus, and jaundice. Labs revealed a direct hyperbilirubinemia with a mixed hepatocellular/cholestatic pattern of liver injury. Tumor markers (CA-19-9, CA-125, CEA, AFP) were normal. CT of abdomen/pelvis reported a 3.7 cm hypo-enhancing pancreatic head mass with biliary and pancreatic duct obstruction associated with lymphadenopathy (A). Endoscopic ultrasound (EUS) revealed an irregular 30 mm x 21 mm hypoechoic, solid irregular mass in the pancreatic head with surrounding peripancreatic lymphadenopathy (C, D). Fine needle aspirate (FNA) revealed a CD138+ plasma cell rich smear with positive Lamba in-situ hybridization stain (ISH) and negative Kappa ISH confirming a malignant plasma cell neoplasm (E-H). On Endoscopic Retrograde Cholangiopancreatography, the common bile duct was dilated with a stricture noted within the intrapancreatic portion at the pancreatic head (C, D). Sphincterotomy was performed and a covered metal stent was placed. The jaundice and pruritus resolved, however repeat imaging two weeks later demonstrated significant interval growth of the mass and the patient succumbed to his illness within six weeks of diagnosis (B).
Discussion: Our case demonstrates the importance of considering extramedullary plasmacytoma when a patient with MM presents with a pancreatic mass, particularly one showing a rapid interval growth, which is not typically seen with primary pancreatic parenchymal diseases such as cancer, cysts, etc. Focal involvement of the head of the pancreas is typical, but diffuse involvement has been reported. Radiographic and lab findings are non-specific, and tumor markers are usually normal, which aids in suggesting a hemopoietic etiology. Definitive diagnosis is best achieved with EUS guided biopsy and immunostaining (E-H). Treatment options include chemotherapy, immunotherapy, or radiation. However, the prognosis remains poor.

Disclosures:
Rehan Razzaq, DO1, Yasra Badi, MD2, Mahum Nadeem, MBBS3, Asiya Tafader, MBBS3, Joseph S.. Spataro, MD4. P0062 - Pancreatic Plasmacytoma Presenting as Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Virginia Commonwealth University, Richmond, VA; 2HCA MountainView Hospital, Arlington, VA; 3Virginia Commonwealth University, Henrico, VA; 4Hunter Holmes Mcguire VA, Richmond, VA
Introduction: Extramedullary solitary plasmacytomas are an uncommon manifestation of plasma cell disorders. It is associated with a poor prognosis with a median survival rate of less than six months. Although rare to involve the digestive tract, the liver is the most common site, with pancreatic involvement demonstrating a 2.3% incidence rate. We report a case of pancreatic plasmacytoma in a patient with multiple myeloma (MM) presenting with painless obstructive jaundice.
Case Description/Methods: An 84-year-old male with a history of MM and cutaneous plasmacytomas presented with a three-week onset of acholic stool, pruritus, and jaundice. Labs revealed a direct hyperbilirubinemia with a mixed hepatocellular/cholestatic pattern of liver injury. Tumor markers (CA-19-9, CA-125, CEA, AFP) were normal. CT of abdomen/pelvis reported a 3.7 cm hypo-enhancing pancreatic head mass with biliary and pancreatic duct obstruction associated with lymphadenopathy (A). Endoscopic ultrasound (EUS) revealed an irregular 30 mm x 21 mm hypoechoic, solid irregular mass in the pancreatic head with surrounding peripancreatic lymphadenopathy (C, D). Fine needle aspirate (FNA) revealed a CD138+ plasma cell rich smear with positive Lamba in-situ hybridization stain (ISH) and negative Kappa ISH confirming a malignant plasma cell neoplasm (E-H). On Endoscopic Retrograde Cholangiopancreatography, the common bile duct was dilated with a stricture noted within the intrapancreatic portion at the pancreatic head (C, D). Sphincterotomy was performed and a covered metal stent was placed. The jaundice and pruritus resolved, however repeat imaging two weeks later demonstrated significant interval growth of the mass and the patient succumbed to his illness within six weeks of diagnosis (B).
Discussion: Our case demonstrates the importance of considering extramedullary plasmacytoma when a patient with MM presents with a pancreatic mass, particularly one showing a rapid interval growth, which is not typically seen with primary pancreatic parenchymal diseases such as cancer, cysts, etc. Focal involvement of the head of the pancreas is typical, but diffuse involvement has been reported. Radiographic and lab findings are non-specific, and tumor markers are usually normal, which aids in suggesting a hemopoietic etiology. Definitive diagnosis is best achieved with EUS guided biopsy and immunostaining (E-H). Treatment options include chemotherapy, immunotherapy, or radiation. However, the prognosis remains poor.

Figure: CT revealed (A) A 33.4mm x 37.4mm hypo-enhancing pancreatic head mass (B ) CT two weeks later shows significant interval growth of hypo-enhancing pancreatic head mass to 50.0mm x 57.1mm.
ERCP revealed (C) A dilated common bile duct to 15mm in diameter (D) Diffuse intrahepatic biliary duct dilatation.
Histology shows (E) Scattered lymphoid cells with a predominance of plasma cells in nests (F) CD138 positivity confirming presence of plasma cells (G) Lamba In-situ hybridization positive stain and (H)- Kappa In-situ hybridization negative stain signifying a monoclonal or malignant population of plasma cells
ERCP revealed (C) A dilated common bile duct to 15mm in diameter (D) Diffuse intrahepatic biliary duct dilatation.
Histology shows (E) Scattered lymphoid cells with a predominance of plasma cells in nests (F) CD138 positivity confirming presence of plasma cells (G) Lamba In-situ hybridization positive stain and (H)- Kappa In-situ hybridization negative stain signifying a monoclonal or malignant population of plasma cells
Disclosures:
Rehan Razzaq indicated no relevant financial relationships.
Yasra Badi indicated no relevant financial relationships.
Mahum Nadeem indicated no relevant financial relationships.
Asiya Tafader indicated no relevant financial relationships.
Joseph Spataro indicated no relevant financial relationships.
Rehan Razzaq, DO1, Yasra Badi, MD2, Mahum Nadeem, MBBS3, Asiya Tafader, MBBS3, Joseph S.. Spataro, MD4. P0062 - Pancreatic Plasmacytoma Presenting as Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
