Sunday Poster Session
Category: Biliary/Pancreas
P0068 - Intra-Articular Steroid Injection as the Etiology of Acute Pancreatitis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- SA
Sareena Ali, DO
Advocate Lutheran General Hospital
Park Ridge, IL
Presenting Author(s)
Sareena Ali, DO, Alan Shapiro, MD, FACG
Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Acute pancreatitis is characterized by inflammation of the pancreatic parenchyma, resulting in mild to severe epigastric pain. Etiologies most commonly include gallstones and alcohol use, while less common causes are infection, autoimmune, and drug-induced. Corticosteroids are a known cause of drug-induced pancreatitis. We present a unique case of recurrent pancreatitis after intra-articular corticosteroid injections.
Case Description/Methods: A 53 year old male with a history of eosinophilic esophagitis (EoE) developed acute epigastric pain three days after injection of betamethasone into his right shoulder. He had been on chronic oral budesonide for EoE, but there were no new oral medications. He had a prior cholecystectomy and infrequent alcohol use. Amylase and lipase were elevated to 136 U/L and 1,668 U/L, respectively. CRP was elevated to 31.4 mg/L. Liver function tests were normal. MRCP showed findings consistent with mild acute interstitial pancreatitis, a 7 mm pancreatic cyst, no pancreatic or biliary ductal dilatation, and no choledocholithiasis. IgG4 level was normal at 48 mg/dL and triglycerides were 130 mg/dL. EGD with EUS showed normal parenchyma of the pancreas without any mass lesion and a non-dilated pancreatic duct. Pancreatitis resolved without hospitalization or need for narcotics, and the etiology of pancreatitis was not determined. Two years later, the patient again presented with epigastric pain three days after receiving a betamethasone injection in his left shoulder. Lipase was 5,624 U/L and MRCP again showed mild interstitial pancreatitis with normal bile ducts, no pancreas divisum, and stable cystic foci in the pancreas. His epigastric pain lasted for about three days, and he did not require hospitalization.
Discussion: To our knowledge, this is only the second reported case of recurrent pancreatitis due to an intra-articular cortisone injection. There is also a reported case of pancreatitis after lumbar epidural steroid injection. In our patient, other etiologies of pancreatitis were ruled out and the temporal relationship between intra-articular steroid injection and development of pancreatitis, on two separate occasions, makes the betamethasone injection the likely etiology. Therefore, we suggest adding intra-articular steroids to the list of etiologies of drug-induced pancreatitis. Consideration should be given to include pancreatitis as a possible adverse effect when obtaining informed consent for local steroid injections.

Disclosures:
Sareena Ali, DO, Alan Shapiro, MD, FACG. P0068 - Intra-Articular Steroid Injection as the Etiology of Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Acute pancreatitis is characterized by inflammation of the pancreatic parenchyma, resulting in mild to severe epigastric pain. Etiologies most commonly include gallstones and alcohol use, while less common causes are infection, autoimmune, and drug-induced. Corticosteroids are a known cause of drug-induced pancreatitis. We present a unique case of recurrent pancreatitis after intra-articular corticosteroid injections.
Case Description/Methods: A 53 year old male with a history of eosinophilic esophagitis (EoE) developed acute epigastric pain three days after injection of betamethasone into his right shoulder. He had been on chronic oral budesonide for EoE, but there were no new oral medications. He had a prior cholecystectomy and infrequent alcohol use. Amylase and lipase were elevated to 136 U/L and 1,668 U/L, respectively. CRP was elevated to 31.4 mg/L. Liver function tests were normal. MRCP showed findings consistent with mild acute interstitial pancreatitis, a 7 mm pancreatic cyst, no pancreatic or biliary ductal dilatation, and no choledocholithiasis. IgG4 level was normal at 48 mg/dL and triglycerides were 130 mg/dL. EGD with EUS showed normal parenchyma of the pancreas without any mass lesion and a non-dilated pancreatic duct. Pancreatitis resolved without hospitalization or need for narcotics, and the etiology of pancreatitis was not determined. Two years later, the patient again presented with epigastric pain three days after receiving a betamethasone injection in his left shoulder. Lipase was 5,624 U/L and MRCP again showed mild interstitial pancreatitis with normal bile ducts, no pancreas divisum, and stable cystic foci in the pancreas. His epigastric pain lasted for about three days, and he did not require hospitalization.
Discussion: To our knowledge, this is only the second reported case of recurrent pancreatitis due to an intra-articular cortisone injection. There is also a reported case of pancreatitis after lumbar epidural steroid injection. In our patient, other etiologies of pancreatitis were ruled out and the temporal relationship between intra-articular steroid injection and development of pancreatitis, on two separate occasions, makes the betamethasone injection the likely etiology. Therefore, we suggest adding intra-articular steroids to the list of etiologies of drug-induced pancreatitis. Consideration should be given to include pancreatitis as a possible adverse effect when obtaining informed consent for local steroid injections.

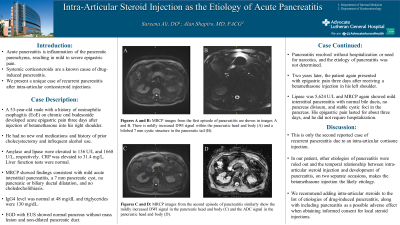
Figure: MRCP images from the first episode of pancreatitis are shown in images A and B. There is the mildly increased DWI signal within the pancreatic head and body (A) and a bilobed 7 mm cystic structure in the pancreatic tail (B). MRCP images from the second episode of pancreatitis similarly show the mildly increased DWI signal in the pancreatic head and body (C) and the ADC signal in the pancreatic head and body (D).
Disclosures:
Sareena Ali indicated no relevant financial relationships.
Alan Shapiro indicated no relevant financial relationships.
Sareena Ali, DO, Alan Shapiro, MD, FACG. P0068 - Intra-Articular Steroid Injection as the Etiology of Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

