Sunday Poster Session
Category: Biliary/Pancreas
P0069 - Extramedullary Multiple Myeloma Causing Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- SA
Sareena Ali, DO
Advocate Lutheran General Hospital
Park Ridge, IL
Presenting Author(s)
Sareena Ali, DO, Saad Hashmi, MD, Nahren Asado, MD, Julio Cabrera, MD, Baseer Qazi, MD
Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Multiple myeloma (MM) is a malignant proliferation of plasma cells in the bone marrow which produce a large quantity of an immunoglobulin. Extramedullary spread to the gastrointestinal (GI) tract is rare and indicates a poor prognosis. We report a unique case of MM in a patient who was refractory to standard and salvage therapy, status post chimeric antigen receptor (CAR) T-cell therapy, presenting with obstructive jaundice from plasmacytoma.
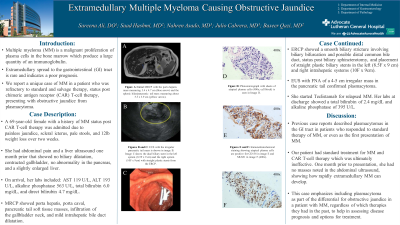
Case Description/Methods: A 69 year old female with a history of MM status post CAR T-cell therapy was admitted due to jaundice. She had abdominal pain and a liver ultrasound one month prior to presenting that showed no biliary dilatation, contracted gallbladder, no abnormality in the pancreas, and a slightly enlarged liver. Upon presentation to our hospital, she had painless jaundice and noted scleral icterus three days prior to admission. She had pale stools and poor appetite over two weeks, causing a 12 lb weight loss. On arrival, her labs included: AST 119 U/L, ALT 193 U/L, alkaline phosphatase 563 U/L, total bilirubin 6.0 mg/dL, and direct bilirubin 4.7 mg/dL. MRCP showed porta hepatis, portacaval, pancreatic tail soft tissue masses, infiltration of the gallbladder neck, and mild intrahepatic bile duct dilatation. ERCP showed a smooth biliary stricture involving biliary bifurcation and possible distal common bile duct, status post biliary sphincterotomy, and placement of straight plastic biliary stents in the left (8.5F x 9 cm) and right intrahepatic systems (10F x 9cm). EUS with FNA of a 4-5 cm irregular mass in the pancreatic tail confirmed plasmacytoma. She started Teclistamab for relapsed MM. Her labs at discharge showed a total bilirubin of 2.4 mg/dL and alkaline phosphatase of 395 U/L.
Discussion: Our patient had extramedullary MM spreading to the GI tract, causing jaundice. Previous case reports described plasmacytomas in the GI tract in patients who responded to standard therapy of MM, or even as the first presentation of MM. Our patient had standard treatment for MM and CAR T-cell therapy which was ultimately ineffective. One month prior to presentation, she had abdominal pain without signs of obstructive jaundice or masses noted in the abdominal ultrasound, showing how rapidly extramedullary MM can develop. This case emphasizes including plasmacytoma as part of the differential for obstructive jaundice in a patient with MM, regardless of which therapies they had in the past, to help in assessing disease prognosis and options for treatment.

Disclosures:
Sareena Ali, DO, Saad Hashmi, MD, Nahren Asado, MD, Julio Cabrera, MD, Baseer Qazi, MD. P0069 - Extramedullary Multiple Myeloma Causing Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Multiple myeloma (MM) is a malignant proliferation of plasma cells in the bone marrow which produce a large quantity of an immunoglobulin. Extramedullary spread to the gastrointestinal (GI) tract is rare and indicates a poor prognosis. We report a unique case of MM in a patient who was refractory to standard and salvage therapy, status post chimeric antigen receptor (CAR) T-cell therapy, presenting with obstructive jaundice from plasmacytoma.
Case Description/Methods: A 69 year old female with a history of MM status post CAR T-cell therapy was admitted due to jaundice. She had abdominal pain and a liver ultrasound one month prior to presenting that showed no biliary dilatation, contracted gallbladder, no abnormality in the pancreas, and a slightly enlarged liver. Upon presentation to our hospital, she had painless jaundice and noted scleral icterus three days prior to admission. She had pale stools and poor appetite over two weeks, causing a 12 lb weight loss. On arrival, her labs included: AST 119 U/L, ALT 193 U/L, alkaline phosphatase 563 U/L, total bilirubin 6.0 mg/dL, and direct bilirubin 4.7 mg/dL. MRCP showed porta hepatis, portacaval, pancreatic tail soft tissue masses, infiltration of the gallbladder neck, and mild intrahepatic bile duct dilatation. ERCP showed a smooth biliary stricture involving biliary bifurcation and possible distal common bile duct, status post biliary sphincterotomy, and placement of straight plastic biliary stents in the left (8.5F x 9 cm) and right intrahepatic systems (10F x 9cm). EUS with FNA of a 4-5 cm irregular mass in the pancreatic tail confirmed plasmacytoma. She started Teclistamab for relapsed MM. Her labs at discharge showed a total bilirubin of 2.4 mg/dL and alkaline phosphatase of 395 U/L.
Discussion: Our patient had extramedullary MM spreading to the GI tract, causing jaundice. Previous case reports described plasmacytomas in the GI tract in patients who responded to standard therapy of MM, or even as the first presentation of MM. Our patient had standard treatment for MM and CAR T-cell therapy which was ultimately ineffective. One month prior to presentation, she had abdominal pain without signs of obstructive jaundice or masses noted in the abdominal ultrasound, showing how rapidly extramedullary MM can develop. This case emphasizes including plasmacytoma as part of the differential for obstructive jaundice in a patient with MM, regardless of which therapies they had in the past, to help in assessing disease prognosis and options for treatment.

Figure: Figure 1: Image A shows the initial MRCP with the porta hepatis mass measuring 3.4 x 4.7 cm (blue arrow) and the splenic hilar/pancreatic tail mass measuring about 5.3 x 3.9 cm (yellow arrow). EUS with the irregular pancreatic tail mass is shown in image B. Image C shows the dual biliary stent in the left system (8.5F x 9 cm) and the right system (10F x 9cm) with straight plastic stents from the ERCP. Photomicrograph with sheets of atypical plasma cells (400x; cell block) is seen in Image D. Immunohistochemical staining showing atypical plasma cells are positive for CD138 in image E and MUM1 in image F (400x).
Disclosures:
Sareena Ali indicated no relevant financial relationships.
Saad Hashmi indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Julio Cabrera indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Sareena Ali, DO, Saad Hashmi, MD, Nahren Asado, MD, Julio Cabrera, MD, Baseer Qazi, MD. P0069 - Extramedullary Multiple Myeloma Causing Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
