Sunday Poster Session
Category: Biliary/Pancreas
P0070 - Acute Pancreatitis Due to Semaglutide: Another Medication to Worry About!
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- FP
Femina Patel, MD
University of California Riverside
San Bernardino, CA
Presenting Author(s)
Arnold Gan, MD1, Femina Patel, MD2, Karen Chang, DO2, Kenneth J. Vega, MD, FACG3
1University of California Riverside, Riverside, CA; 2University of California Riverside, San Bernardino, CA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Reports of acute pancreatitis secondary to subcutaneous semaglutide, a medication commonly used in antidiabetic regimens and marketed for weight loss, is exceedingly rare. This leads to its routine exclusion from a comprehensive differential diagnosis during the initial workup of acute pancreatitis and delayed intervention.
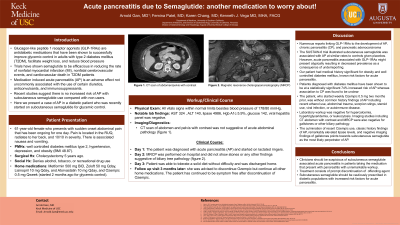
Case Description/Methods: A 61-year-old female with past medical history of diabetes mellitus type 2, hypertension, depression, morbid obesity and cholecystectomy 5 years prior presented to the emergency room with one day of sudden onset of severe right upper quadrant pain with radiation to the back, nausea and non-bilious non-bloody vomiting. There was no history of alcohol use, tobacco use, illicit drug use, or recent abdominal trauma. Current medications were metformin 500 mg daily, zolpidem 50 mg daily, lisinopril 10 mg daily, atorvastatin 500 mg twice daily by mouth along with 0.5 mg subcutaneous semaglutide once weekly (started two months prior to presentation). All vital signs were within normal limits other than an elevated blood pressure of 178/80 mmHg. Physical exam revealed severe epigastric tenderness to palpation. Laboratory data was significant for aspartate aminotransferase of 324, alanine aminotransferase of 140 and lipase notably elevated at 4,936. Computed tomography of the abdomen and pelvis with intravenous contrast revealed no acute abnormality (Fig 1A). Based on exam and elevated lipase levels, the patient was diagnosed with acute pancreatitis. Magnetic resonance cholangiopancreatography performed on hospital day 2 revealed no obstructive stones or any findings suggestive of biliary tree pathology (Fig 1B). The following day, the patient tolerated a solid diet and was advised not to restart subcutaneous semaglutide upon discharge. She remained symptom-free at follow-up visit three months later post hospitalization.
Discussion: Subcutaneous semaglutide is becoming more favored among diabetics for glycemic control. This case suggests, although rare, subcutaneous semaglutide should remain on a clinician’s differential diagnosis as a drug induced etiology when evaluating acute pancreatitis. Recognition of this can lead to early diagnosis, discontinuation of the offending agent, and expedited recovery.

Disclosures:
Arnold Gan, MD1, Femina Patel, MD2, Karen Chang, DO2, Kenneth J. Vega, MD, FACG3. P0070 - Acute Pancreatitis Due to Semaglutide: Another Medication to Worry About!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California Riverside, Riverside, CA; 2University of California Riverside, San Bernardino, CA; 3Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Reports of acute pancreatitis secondary to subcutaneous semaglutide, a medication commonly used in antidiabetic regimens and marketed for weight loss, is exceedingly rare. This leads to its routine exclusion from a comprehensive differential diagnosis during the initial workup of acute pancreatitis and delayed intervention.
Case Description/Methods: A 61-year-old female with past medical history of diabetes mellitus type 2, hypertension, depression, morbid obesity and cholecystectomy 5 years prior presented to the emergency room with one day of sudden onset of severe right upper quadrant pain with radiation to the back, nausea and non-bilious non-bloody vomiting. There was no history of alcohol use, tobacco use, illicit drug use, or recent abdominal trauma. Current medications were metformin 500 mg daily, zolpidem 50 mg daily, lisinopril 10 mg daily, atorvastatin 500 mg twice daily by mouth along with 0.5 mg subcutaneous semaglutide once weekly (started two months prior to presentation). All vital signs were within normal limits other than an elevated blood pressure of 178/80 mmHg. Physical exam revealed severe epigastric tenderness to palpation. Laboratory data was significant for aspartate aminotransferase of 324, alanine aminotransferase of 140 and lipase notably elevated at 4,936. Computed tomography of the abdomen and pelvis with intravenous contrast revealed no acute abnormality (Fig 1A). Based on exam and elevated lipase levels, the patient was diagnosed with acute pancreatitis. Magnetic resonance cholangiopancreatography performed on hospital day 2 revealed no obstructive stones or any findings suggestive of biliary tree pathology (Fig 1B). The following day, the patient tolerated a solid diet and was advised not to restart subcutaneous semaglutide upon discharge. She remained symptom-free at follow-up visit three months later post hospitalization.
Discussion: Subcutaneous semaglutide is becoming more favored among diabetics for glycemic control. This case suggests, although rare, subcutaneous semaglutide should remain on a clinician’s differential diagnosis as a drug induced etiology when evaluating acute pancreatitis. Recognition of this can lead to early diagnosis, discontinuation of the offending agent, and expedited recovery.

Figure: FIG-1A: Computed tomography (CT) scan of the abdomen and pelvis with contrast showed no pancreatic pathology. Figure 1B: Magnetic resonance cholangiopancreatography (MRCP) showing a normal caliber common bile duct, pancreatic duct, and a remnant cystic duct status post cholecystectomy.
Disclosures:
Arnold Gan indicated no relevant financial relationships.
Femina Patel indicated no relevant financial relationships.
Karen Chang indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Arnold Gan, MD1, Femina Patel, MD2, Karen Chang, DO2, Kenneth J. Vega, MD, FACG3. P0070 - Acute Pancreatitis Due to Semaglutide: Another Medication to Worry About!, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
