Sunday Poster Session
Category: Biliary/Pancreas
P0075 - Time, Nature's Duct Tape: Nonoperative Management of a Common Hepatic Duct Perforation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Andrew Mertz, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Andrew Mertz, MD1, Ashley Humphries, MD1, William Parker, MD2, Emad Madha, MD1, Jeffrey Laczek, MD1
1Walter Reed National Military Medical Center, Bethesda, MD; 2Naval Medical Center, Camp Lejeune, NC
Introduction: Cholecystobiliary fistulas are a complication of Mirizzi syndrome, an uncommon condition caused by external compression of the common hepatic duct (CHD) by a gallstone. Surgical repair of a cholecystobiliary fistula generally requires hepaticojejunostomy. Herein, we describe a case of cholecystobiliary fistula with resultant CHD defect that resolved with nonoperatively management.
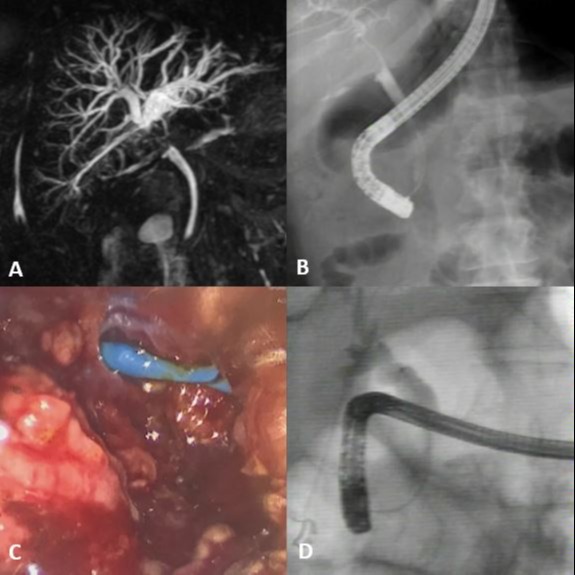
Case Description/Methods: A 65-year-old man presented with right upper quadrant pain. Labs revealed elevated liver chemistries in a cholestatic pattern and cross-sectional imaging revealed external compression of the CHD by a stone in the gallbladder neck. He underwent endoscopic retrograde cholangiopancreatography (ERCP) which showed extrinsic compression of the CHD without choledocholithiasis. There was no clear evidence of a cholecystobiliary fistula and a biliary stent was placed. The patient subsequently underwent a laparoscopic subtotal cholecystectomy due to a gangrenous gallbladder with significant adhesions to the surrounding tissue. Upon removal of the largest gallstone, the biliary stent was visualized through a hemi-circumfrential defect in the CHD, consistent with a cholecystobiliary fistula, and a drain was placed in the gallbladder fossa. Large amounts of bilious drain output continued postoperatively and the patient was referred for a hepaticojejunostomy. While waiting for his nutritional and functional status to improve prior to surgery, his biliary stents and external drains were exchanged multiple times with ongoing high output from the drain. All the while, the patient reported minimal symptoms. A contrast external drain study showed a small cavity adjacent to and communicating with the CHD. Following this study, the patient’s drain was downsized and later inadvertently removed. The drain was not replaced and the patient continued to have minimal symptoms. A final ERCP showed a small outpouching at the site of the previous CHD defect; the patient’s biliary stent was removed and the patient has continued to do well for over a year.
Discussion: Cholecystobiliary fistulas are challenging to manage and typically require multi-disciplinary treatment. In our patient, the resultant hemi-circumferential perforation was managed nonoperatively and ultimately created a walled-off cavity that allowed the patient to avoid surgery. This case highlights that a combination of endoscopic and percutaneous treatments may obviate the need for a major surgery to repair this defect.
Disclosures:
Andrew Mertz, MD1, Ashley Humphries, MD1, William Parker, MD2, Emad Madha, MD1, Jeffrey Laczek, MD1. P0075 - Time, Nature's Duct Tape: Nonoperative Management of a Common Hepatic Duct Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2Naval Medical Center, Camp Lejeune, NC
Introduction: Cholecystobiliary fistulas are a complication of Mirizzi syndrome, an uncommon condition caused by external compression of the common hepatic duct (CHD) by a gallstone. Surgical repair of a cholecystobiliary fistula generally requires hepaticojejunostomy. Herein, we describe a case of cholecystobiliary fistula with resultant CHD defect that resolved with nonoperatively management.
Case Description/Methods: A 65-year-old man presented with right upper quadrant pain. Labs revealed elevated liver chemistries in a cholestatic pattern and cross-sectional imaging revealed external compression of the CHD by a stone in the gallbladder neck. He underwent endoscopic retrograde cholangiopancreatography (ERCP) which showed extrinsic compression of the CHD without choledocholithiasis. There was no clear evidence of a cholecystobiliary fistula and a biliary stent was placed. The patient subsequently underwent a laparoscopic subtotal cholecystectomy due to a gangrenous gallbladder with significant adhesions to the surrounding tissue. Upon removal of the largest gallstone, the biliary stent was visualized through a hemi-circumfrential defect in the CHD, consistent with a cholecystobiliary fistula, and a drain was placed in the gallbladder fossa. Large amounts of bilious drain output continued postoperatively and the patient was referred for a hepaticojejunostomy. While waiting for his nutritional and functional status to improve prior to surgery, his biliary stents and external drains were exchanged multiple times with ongoing high output from the drain. All the while, the patient reported minimal symptoms. A contrast external drain study showed a small cavity adjacent to and communicating with the CHD. Following this study, the patient’s drain was downsized and later inadvertently removed. The drain was not replaced and the patient continued to have minimal symptoms. A final ERCP showed a small outpouching at the site of the previous CHD defect; the patient’s biliary stent was removed and the patient has continued to do well for over a year.
Discussion: Cholecystobiliary fistulas are challenging to manage and typically require multi-disciplinary treatment. In our patient, the resultant hemi-circumferential perforation was managed nonoperatively and ultimately created a walled-off cavity that allowed the patient to avoid surgery. This case highlights that a combination of endoscopic and percutaneous treatments may obviate the need for a major surgery to repair this defect.
Figure: A) MRCP reconstruction demonstrating compression at the level of the common hepatic duct from cholelith at gallbladder neck
B) Cholangiogram demonstrating filling defect at level of common hepatic duct, potentially some contrast seen in gallbladder fossa
C) Biliary stent seen laparoscopically after disimpaction of stone at gallbladder neck leading to common hepatic perforation
D) Follow-up cholangiogram revealing small outpouching at the site of the previous common hepatic duct defect
B) Cholangiogram demonstrating filling defect at level of common hepatic duct, potentially some contrast seen in gallbladder fossa
C) Biliary stent seen laparoscopically after disimpaction of stone at gallbladder neck leading to common hepatic perforation
D) Follow-up cholangiogram revealing small outpouching at the site of the previous common hepatic duct defect
Disclosures:
Andrew Mertz indicated no relevant financial relationships.
Ashley Humphries indicated no relevant financial relationships.
William Parker indicated no relevant financial relationships.
Emad Madha indicated no relevant financial relationships.
Jeffrey Laczek indicated no relevant financial relationships.
Andrew Mertz, MD1, Ashley Humphries, MD1, William Parker, MD2, Emad Madha, MD1, Jeffrey Laczek, MD1. P0075 - Time, Nature's Duct Tape: Nonoperative Management of a Common Hepatic Duct Perforation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
