Monday Poster Session
Category: Esophagus
P1815 - Esophagogastroduodenoscopy Plays an Important Preoperative Role in Bariatric Surgery: Systematic Review and Meta-Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rami Musallam, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Azizullah Beran, MD4, Babu Mohan, MD, MS5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Pearl Aggarwal, MD8, Emad Mansoor, MD9, Mohannad Abousaleh, MD10, C. Roberto Simons-Linares, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD11
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cleveland Clinic Akron General, Akron, OH; 4Indiana University, Indianapolis, IN; 5University of Utah Health School of Medicine, Salt Lake City, UT; 6Oakland University William Beaumont School of Medicine, Farmington Hills, MI; 7University of Toledo, Toledo, OH; 8University Hospitals St. John Medical Center, Westlake, OH; 9Case Western Reserve University / University Hospitals, Cleveland, OH; 10Huron Gastroenterology, Ann Arbor, MI; 11Cleveland Clinic, Cleveland, OH; 12Case Western Reserve/UHCMC, Cleveland, OH
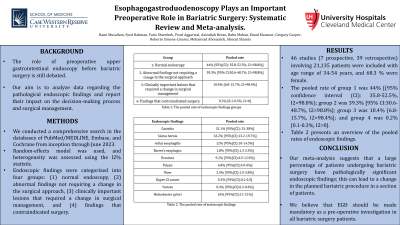
Introduction: The role of preoperative upper gastrointestinal endoscopy before bariatric surgery is still debated, and a consensus among the international scientific community is lacking. Our aim is to analyze data regarding the pathological endoscopic findings and report their impact on the decision-making process and surgical management, in terms of delay in surgical operation, modification of the intended bariatric procedure, or contraindication to surgery.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through June 2023. Meta-analysis was performed by standard methodology using the random-effects model and heterogeneity was assessed using the I2% statistics. Endoscopic findings were categorized into four groups: (1) normal endoscopy, (2) abnormal findings not requiring a change in the surgical approach, (3) clinically important lesions that required a change in surgical management or further investigations or therapy prior to surgery, and (4) findings that contraindicated surgery.
Results: 46 studies (7 prospective, 39 retrospective) involving 21,135 patients were included with age range of 34-54 years, and 68.3 % were female. The pooled rate of group 1 was 44% [(95% confidence interval (CI): 35.8-52.5%, I2=98.8%); group 2 was 39.3% [95% CI:30.6-48.7%, I2=98.8%]; group 3 was 10.4% [6.8-15.7%, I2=98.4%]; and group 4 was 0.2% [0.1-0.3%, I2=0].
Pooled rates of endoscopic findings included gastritis in 31.1% [25-38%] (erosive gastritis in 12%), hiatus hernia in 16.2% [13.2-19.7%] (≥ 3 cm in 22.6%), reflux esophagitis in 12% [10-14.5%] (15.8% grade B and C), Barret’s esophagus in 1.8% [1.3-2.5%], erosions in 9.2% [6.5-12.9%], polyps 4.8% [3.9-6%], ulcer in 2.4% [1.5-3.8%], upper GI cancer in 0.3% [0.2-0.5], varices in 0.3% [0.2-0.6%] and Helicobacter pylori in 16% [12-21%]. No evidence of publication bias was found (Egger’s test: P=0.11).
Discussion: Our meta-analysis suggests that a large percentage of patients undergoing bariatric surgery have pathologically significant endoscopic findings; this can lead to a change in the planned bariatric procedure in a section of patients; hence, we believe that EGD should be made mandatory as a pre-operative investigation in all bariatric surgery patients. A randomized trial should be performed to validate the usefulness of preoperative EGD in bariatric patients.
Disclosures:
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Azizullah Beran, MD4, Babu Mohan, MD, MS5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Pearl Aggarwal, MD8, Emad Mansoor, MD9, Mohannad Abousaleh, MD10, C. Roberto Simons-Linares, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD11. P1815 - Esophagogastroduodenoscopy Plays an Important Preoperative Role in Bariatric Surgery: Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cleveland Clinic Akron General, Akron, OH; 4Indiana University, Indianapolis, IN; 5University of Utah Health School of Medicine, Salt Lake City, UT; 6Oakland University William Beaumont School of Medicine, Farmington Hills, MI; 7University of Toledo, Toledo, OH; 8University Hospitals St. John Medical Center, Westlake, OH; 9Case Western Reserve University / University Hospitals, Cleveland, OH; 10Huron Gastroenterology, Ann Arbor, MI; 11Cleveland Clinic, Cleveland, OH; 12Case Western Reserve/UHCMC, Cleveland, OH
Introduction: The role of preoperative upper gastrointestinal endoscopy before bariatric surgery is still debated, and a consensus among the international scientific community is lacking. Our aim is to analyze data regarding the pathological endoscopic findings and report their impact on the decision-making process and surgical management, in terms of delay in surgical operation, modification of the intended bariatric procedure, or contraindication to surgery.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through June 2023. Meta-analysis was performed by standard methodology using the random-effects model and heterogeneity was assessed using the I2% statistics. Endoscopic findings were categorized into four groups: (1) normal endoscopy, (2) abnormal findings not requiring a change in the surgical approach, (3) clinically important lesions that required a change in surgical management or further investigations or therapy prior to surgery, and (4) findings that contraindicated surgery.
Results: 46 studies (7 prospective, 39 retrospective) involving 21,135 patients were included with age range of 34-54 years, and 68.3 % were female. The pooled rate of group 1 was 44% [(95% confidence interval (CI): 35.8-52.5%, I2=98.8%); group 2 was 39.3% [95% CI:30.6-48.7%, I2=98.8%]; group 3 was 10.4% [6.8-15.7%, I2=98.4%]; and group 4 was 0.2% [0.1-0.3%, I2=0].
Pooled rates of endoscopic findings included gastritis in 31.1% [25-38%] (erosive gastritis in 12%), hiatus hernia in 16.2% [13.2-19.7%] (≥ 3 cm in 22.6%), reflux esophagitis in 12% [10-14.5%] (15.8% grade B and C), Barret’s esophagus in 1.8% [1.3-2.5%], erosions in 9.2% [6.5-12.9%], polyps 4.8% [3.9-6%], ulcer in 2.4% [1.5-3.8%], upper GI cancer in 0.3% [0.2-0.5], varices in 0.3% [0.2-0.6%] and Helicobacter pylori in 16% [12-21%]. No evidence of publication bias was found (Egger’s test: P=0.11).
Discussion: Our meta-analysis suggests that a large percentage of patients undergoing bariatric surgery have pathologically significant endoscopic findings; this can lead to a change in the planned bariatric procedure in a section of patients; hence, we believe that EGD should be made mandatory as a pre-operative investigation in all bariatric surgery patients. A randomized trial should be performed to validate the usefulness of preoperative EGD in bariatric patients.
Disclosures:
Rami Musallam indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Faris Shweikeh indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Rania Daaboul indicated no relevant financial relationships.
Wasef Sayeh indicated no relevant financial relationships.
Pearl Aggarwal indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Mohannad Abousaleh indicated no relevant financial relationships.
C. Roberto Simons-Linares indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Ahmed Shamia indicated no relevant financial relationships.
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Azizullah Beran, MD4, Babu Mohan, MD, MS5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Pearl Aggarwal, MD8, Emad Mansoor, MD9, Mohannad Abousaleh, MD10, C. Roberto Simons-Linares, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD11. P1815 - Esophagogastroduodenoscopy Plays an Important Preoperative Role in Bariatric Surgery: Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
