Monday Poster Session
Category: Esophagus
P1816 - Gastroesophageal Reflux Disease, Esophagitis, and Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rami Musallam, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Alexis Bennett, MD4, Azizullah Beran, MD5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Babu Mohan, MD, MS8, Mohannad Abousaleh, MD9, C. Roberto Simons-Linares, MD10, Emad Mansoor, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD10
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cleveland Clinic Akron General, Akron, OH; 4Case Western Reserve University/Cleveland Medical Center, Cleveland, OH; 5Indiana University, Indianapolis, IN; 6Oakland University William Beaumont School of Medicine, Farmington Hills, MI; 7University of Toledo, Toledo, OH; 8University of Utah Health School of Medicine, Salt Lake City, UT; 9Huron Gastroenterology, Ann Arbor, MI; 10Cleveland Clinic, Cleveland, OH; 11Case Western Reserve University / University Hospitals, Cleveland, OH; 12Case Western Reserve/UHCMC, Cleveland, OH
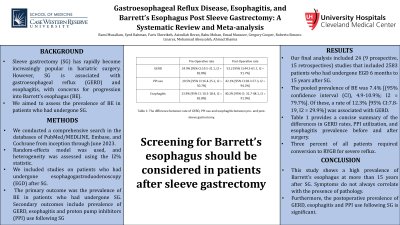
Introduction: Sleeve gastrectomy (SG) has become increasingly popular in bariatric surgery. However, SG is associated with gastroesophageal reflux (GERD) and esophagitis, with concerns for progression into Barrett’s esophagus (BE). We aimed to assess the prevalence of BE in patients who had undergone SG.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through June 2023. Meta-analysis was performed by standard methodology using the random-effects model and heterogeneity was assessed using the I2% statistics. We included studies on patients who had undergone esophagogastroduodenoscopy (EGD) after SG. The primary outcome was the prevalence of BE in patients who had undergone SG. Secondary outcomes include prevalence of GERD, esophagitis and proton pump inhibitors (PPI) use following SG.
Results: Our final analysis included 24 studies (9 prospective, 15 retrospectives) that included 2583 patients who had undergone EGD 6 months to 15 years after SG. The pooled prevalence of BE was 7.4% [(95% confidence interval (CI), 4.9-10.9%; I2 = 79.7%]. Of these, 12.3% [95% CI: 7.8-19, I2 = 29.9%] were associated with GERD. No dysplasia was reported. We found an increase of postoperative GERD after SG with a rate of 53.2% [95% CI: 44.5-61.7, I2 = 91.7%] compared with preoperative rate of 24.9% [95% CI: 19.5-31.1, I2 = 82.8%] and the rate of postoperative esophagitis was 40.2% [95% CI: 32.7-48.1, I2 = 91.9%] compared with preoperative rate of 13.9% [95% CI: 10.3-18.4, I2 = 82.8%]. Moreover, the rate of postoperative PPI use was 42.1% [95% CI: 28.3-57.3, I2 = 94.2%] compared with preoperative rate of 20.5% [95% CI: 16.4-25.2, I2 = 50.7%]. Three percent of all patients required conversion to RYGB for severe reflux.
Discussion: This study shows a high prevalence of Barrett’s esophagus up to 15 years post-SG. Furthermore, the postoperative prevalence of esophagitis, GERD and PPI use almost doubled post-SG. Screening for BE should be considered in all patients after SG.
Disclosures:
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Alexis Bennett, MD4, Azizullah Beran, MD5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Babu Mohan, MD, MS8, Mohannad Abousaleh, MD9, C. Roberto Simons-Linares, MD10, Emad Mansoor, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD10. P1816 - Gastroesophageal Reflux Disease, Esophagitis, and Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland, OH; 2Methodist Dallas Medical Center, Dallas, TX; 3Cleveland Clinic Akron General, Akron, OH; 4Case Western Reserve University/Cleveland Medical Center, Cleveland, OH; 5Indiana University, Indianapolis, IN; 6Oakland University William Beaumont School of Medicine, Farmington Hills, MI; 7University of Toledo, Toledo, OH; 8University of Utah Health School of Medicine, Salt Lake City, UT; 9Huron Gastroenterology, Ann Arbor, MI; 10Cleveland Clinic, Cleveland, OH; 11Case Western Reserve University / University Hospitals, Cleveland, OH; 12Case Western Reserve/UHCMC, Cleveland, OH
Introduction: Sleeve gastrectomy (SG) has become increasingly popular in bariatric surgery. However, SG is associated with gastroesophageal reflux (GERD) and esophagitis, with concerns for progression into Barrett’s esophagus (BE). We aimed to assess the prevalence of BE in patients who had undergone SG.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through June 2023. Meta-analysis was performed by standard methodology using the random-effects model and heterogeneity was assessed using the I2% statistics. We included studies on patients who had undergone esophagogastroduodenoscopy (EGD) after SG. The primary outcome was the prevalence of BE in patients who had undergone SG. Secondary outcomes include prevalence of GERD, esophagitis and proton pump inhibitors (PPI) use following SG.
Results: Our final analysis included 24 studies (9 prospective, 15 retrospectives) that included 2583 patients who had undergone EGD 6 months to 15 years after SG. The pooled prevalence of BE was 7.4% [(95% confidence interval (CI), 4.9-10.9%; I2 = 79.7%]. Of these, 12.3% [95% CI: 7.8-19, I2 = 29.9%] were associated with GERD. No dysplasia was reported. We found an increase of postoperative GERD after SG with a rate of 53.2% [95% CI: 44.5-61.7, I2 = 91.7%] compared with preoperative rate of 24.9% [95% CI: 19.5-31.1, I2 = 82.8%] and the rate of postoperative esophagitis was 40.2% [95% CI: 32.7-48.1, I2 = 91.9%] compared with preoperative rate of 13.9% [95% CI: 10.3-18.4, I2 = 82.8%]. Moreover, the rate of postoperative PPI use was 42.1% [95% CI: 28.3-57.3, I2 = 94.2%] compared with preoperative rate of 20.5% [95% CI: 16.4-25.2, I2 = 50.7%]. Three percent of all patients required conversion to RYGB for severe reflux.
Discussion: This study shows a high prevalence of Barrett’s esophagus up to 15 years post-SG. Furthermore, the postoperative prevalence of esophagitis, GERD and PPI use almost doubled post-SG. Screening for BE should be considered in all patients after SG.
Disclosures:
Rami Musallam indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Faris Shweikeh indicated no relevant financial relationships.
Alexis Bennett indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Rania Daaboul indicated no relevant financial relationships.
Wasef Sayeh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Mohannad Abousaleh indicated no relevant financial relationships.
C. Roberto Simons-Linares indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Ahmed Shamia indicated no relevant financial relationships.
Rami Musallam, MD1, Syed Hamaad Rahman, DO2, Faris Shweikeh, MD3, Alexis Bennett, MD4, Azizullah Beran, MD5, Rania Daaboul, MS6, Wasef Sayeh, MD7, Babu Mohan, MD, MS8, Mohannad Abousaleh, MD9, C. Roberto Simons-Linares, MD10, Emad Mansoor, MD11, Gregory Cooper, MD12, Ahmed Shamia, MD10. P1816 - Gastroesophageal Reflux Disease, Esophagitis, and Barrett’s Esophagus Post Sleeve Gastrectomy: A Systematic Review and Meta-Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
