Monday Poster Session
Category: Esophagus
P1830 - Radiofrequency Ablation During Upper Endoscopy Is Safe in Patients with Permanent Pacemakers
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Thomas J. Wang, MD
Brigham and Women's Hospital
Boston, MA
Presenting Author(s)
Thomas J. Wang, MD1, Kunal Jajoo, MD2
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Boston, MA
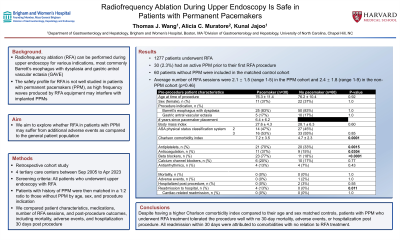
Introduction: Radiofrequency ablation (RFA) can be performed during upper endoscopy for various indications, most commonly Barrett’s esophagus with dysplasia and gastric antral vascular ectasia (GAVE). However, the safety profile for RFA is not well studied in patients with permanent pacemakers (PPM), as high frequency waves produced by RFA equipment may interfere with implanted PPMs. We aimed to explore whether RFA in patients with PPM may suffer from additional adverse events as compared to the general patient population.
Methods: Patients who received RFA treatment during an upper endoscopy were retrospectively identified from an internal Research Patient Data Registry at 4 tertiary care centers between Sep 2005 and Apr 2023. Patient charts were then manually reviewed for history of PPM implantation. Patients with history of PPM were then matched in a 1:2 ratio to those without PPM by age, sex, and procedure indication. We measured and compared patient characteristics, medications, number of RFA sessions, and post-procedure outcomes, which included mortality, adverse events, and hospitalization within 30 days post procedure. Statistics were performed with SAS 9.4 software.
Results: Detailed results are outlined in Table 1. 1277 patients underwent RFA. 30 (2.3%) had an active PPM prior to their first RFA procedure. 60 patients without PPM were included in the matched control cohort. Per matching criteria, the average age was 76.3 and 76.2 for the two cohorts (p=0.92). Both cohorts consisted of 37% female patients, with 83% undergoing RFA for Barrett’s esophagus with dysplasia and 17% for GAVE. Average number of RFA sessions were 2.1 ± 1.5 (range 1-5) in the PPM cohort and 2.4 ± 1.8 (range 1-9) in the non-PPM cohort (p=0.46). The pacemaker cohort had higher average Charlson comorbidity index (7.2 vs 4.7, p=0.0001). 30-day post procedure outcomes were similar, except for all-cause readmissions, which was higher in the PPM group (13 vs 0%, p=0.011). However, none of the causes of readmission were cardiac related. There were no 30-day mortality events in either cohort.
Discussion: Despite having a higher Charlson comorbidity index compared to their age and sex matched controls, patients with PPM who underwent RFA treatment tolerated the procedure well with no 30-day mortality, adverse events, or hospitalization post procedure. All readmission within 30 days were attributed to comorbidities with no relation to RFA treatment.
Disclosures:
Thomas J. Wang, MD1, Kunal Jajoo, MD2. P1830 - Radiofrequency Ablation During Upper Endoscopy Is Safe in Patients with Permanent Pacemakers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Boston, MA
Introduction: Radiofrequency ablation (RFA) can be performed during upper endoscopy for various indications, most commonly Barrett’s esophagus with dysplasia and gastric antral vascular ectasia (GAVE). However, the safety profile for RFA is not well studied in patients with permanent pacemakers (PPM), as high frequency waves produced by RFA equipment may interfere with implanted PPMs. We aimed to explore whether RFA in patients with PPM may suffer from additional adverse events as compared to the general patient population.
Methods: Patients who received RFA treatment during an upper endoscopy were retrospectively identified from an internal Research Patient Data Registry at 4 tertiary care centers between Sep 2005 and Apr 2023. Patient charts were then manually reviewed for history of PPM implantation. Patients with history of PPM were then matched in a 1:2 ratio to those without PPM by age, sex, and procedure indication. We measured and compared patient characteristics, medications, number of RFA sessions, and post-procedure outcomes, which included mortality, adverse events, and hospitalization within 30 days post procedure. Statistics were performed with SAS 9.4 software.
Results: Detailed results are outlined in Table 1. 1277 patients underwent RFA. 30 (2.3%) had an active PPM prior to their first RFA procedure. 60 patients without PPM were included in the matched control cohort. Per matching criteria, the average age was 76.3 and 76.2 for the two cohorts (p=0.92). Both cohorts consisted of 37% female patients, with 83% undergoing RFA for Barrett’s esophagus with dysplasia and 17% for GAVE. Average number of RFA sessions were 2.1 ± 1.5 (range 1-5) in the PPM cohort and 2.4 ± 1.8 (range 1-9) in the non-PPM cohort (p=0.46). The pacemaker cohort had higher average Charlson comorbidity index (7.2 vs 4.7, p=0.0001). 30-day post procedure outcomes were similar, except for all-cause readmissions, which was higher in the PPM group (13 vs 0%, p=0.011). However, none of the causes of readmission were cardiac related. There were no 30-day mortality events in either cohort.
Discussion: Despite having a higher Charlson comorbidity index compared to their age and sex matched controls, patients with PPM who underwent RFA treatment tolerated the procedure well with no 30-day mortality, adverse events, or hospitalization post procedure. All readmission within 30 days were attributed to comorbidities with no relation to RFA treatment.
Disclosures:
Thomas Wang indicated no relevant financial relationships.
Kunal Jajoo indicated no relevant financial relationships.
Thomas J. Wang, MD1, Kunal Jajoo, MD2. P1830 - Radiofrequency Ablation During Upper Endoscopy Is Safe in Patients with Permanent Pacemakers, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
