Monday Poster Session
Category: Esophagus
P1853 - Comprehensive “One-Stop Shop” Esophageal Motility Workup During Propofol Endoscopy: Safe, Feasible, and Convenient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Neil Jariwalla, MD
University of California Irvine
Orange, California
Presenting Author(s)
Neil Jariwalla, MD1, Joshua Kwon, MD1, Amirali Tavangar, MD1, Samuel Ji, MD1, David L. Cheung, MD2, Emily Bernale, BS1, Robert Lee, MD1, Jason Samarasena, MD1
1University of California Irvine, Orange, CA; 2UC Irvine, Orange, CA
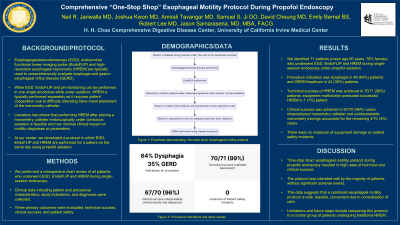
Introduction: In evaluating dysphagia or refractory GERD, patients typically undergo several diagnostic studies including EGD, endoluminal functional lumen imaging probe (EndoFLIP), and high-resolution esophageal manometry (HREM). Endoscopy, EndoFLIP, and pH monitoring can be performed in one single procedure while under sedation. However, HREM is typically performed separately without sedation as it requires patient cooperation. Many patients have difficulty tolerating trans-nasal placement of the manometry catheter. At our center we developed a protocol in which EGD, EndoFLIP, and HREM is performed for a patient on the same day using propofol sedation.
With this protocol, we first perform EGD with EndoFLIP while patients are under monitored anesthesia care or general anesthesia, using only propofol, without use of inhalation agents or paralytics. While asleep, a manometry catheter is placed under endoscopic guidance. Afterwards, the patients are brought to the recovery area where the HRM equipment resides. Once the patient is awake enough to follow commands, they undergo the standard manometry protocol.
Methods: We performed a retrospective review of patients that had undergone EGD/EndoFLIP/HREM during single-session endoscopy. Data collected included detailed patient characteristics, indications for study, and diagnoses. Three main outcome measures were evaluated: Technical success was measured by uncomplicated manometry catheter placement and absence of equipment malfunction, Clinical success was defined by manometry tracing data sufficient for suitable interpretation by a motility specialist and Patient safety
Results: We identified 71 patients (mean age 60, 78% female) who underwent EGD, Endoflip, and HREM during single-session endoscopy under propofol sedation. Procedure indication was dysphagia in 46 (65%) and GERD/heartburn in 24 (34%) of cases. Technical success of HREM was achieved in 70/71 (99%) of patients; equipment malfunction precluded successful HREM in 1 patient. Clinical success was achieved in 67/70 (96%) of cases; mispositioned catheter and uninterpretable manometry tracings accounted for the remaining 3/70 (4%) cases. There were no instances of equipment damage or patient safety incidents.
Discussion: Our study demonstrated that a “one stop shop” esophageal motility protocol during propofol endoscopy was safe, feasible and highly convenient for patients due to consolidation of care and avoidance of unsedated trans-nasal placement of manometry catheters.
Disclosures:
Neil Jariwalla, MD1, Joshua Kwon, MD1, Amirali Tavangar, MD1, Samuel Ji, MD1, David L. Cheung, MD2, Emily Bernale, BS1, Robert Lee, MD1, Jason Samarasena, MD1. P1853 - Comprehensive “One-Stop Shop” Esophageal Motility Workup During Propofol Endoscopy: Safe, Feasible, and Convenient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2UC Irvine, Orange, CA
Introduction: In evaluating dysphagia or refractory GERD, patients typically undergo several diagnostic studies including EGD, endoluminal functional lumen imaging probe (EndoFLIP), and high-resolution esophageal manometry (HREM). Endoscopy, EndoFLIP, and pH monitoring can be performed in one single procedure while under sedation. However, HREM is typically performed separately without sedation as it requires patient cooperation. Many patients have difficulty tolerating trans-nasal placement of the manometry catheter. At our center we developed a protocol in which EGD, EndoFLIP, and HREM is performed for a patient on the same day using propofol sedation.
With this protocol, we first perform EGD with EndoFLIP while patients are under monitored anesthesia care or general anesthesia, using only propofol, without use of inhalation agents or paralytics. While asleep, a manometry catheter is placed under endoscopic guidance. Afterwards, the patients are brought to the recovery area where the HRM equipment resides. Once the patient is awake enough to follow commands, they undergo the standard manometry protocol.
Methods: We performed a retrospective review of patients that had undergone EGD/EndoFLIP/HREM during single-session endoscopy. Data collected included detailed patient characteristics, indications for study, and diagnoses. Three main outcome measures were evaluated: Technical success was measured by uncomplicated manometry catheter placement and absence of equipment malfunction, Clinical success was defined by manometry tracing data sufficient for suitable interpretation by a motility specialist and Patient safety
Results: We identified 71 patients (mean age 60, 78% female) who underwent EGD, Endoflip, and HREM during single-session endoscopy under propofol sedation. Procedure indication was dysphagia in 46 (65%) and GERD/heartburn in 24 (34%) of cases. Technical success of HREM was achieved in 70/71 (99%) of patients; equipment malfunction precluded successful HREM in 1 patient. Clinical success was achieved in 67/70 (96%) of cases; mispositioned catheter and uninterpretable manometry tracings accounted for the remaining 3/70 (4%) cases. There were no instances of equipment damage or patient safety incidents.
Discussion: Our study demonstrated that a “one stop shop” esophageal motility protocol during propofol endoscopy was safe, feasible and highly convenient for patients due to consolidation of care and avoidance of unsedated trans-nasal placement of manometry catheters.
Disclosures:
Neil Jariwalla indicated no relevant financial relationships.
Joshua Kwon indicated no relevant financial relationships.
Amirali Tavangar indicated no relevant financial relationships.
Samuel Ji indicated no relevant financial relationships.
David Cheung indicated no relevant financial relationships.
Emily Bernale indicated no relevant financial relationships.
Robert Lee indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Advisor or Review Panel Member. Boston Scientific – Consultant. Conmed – Consultant. Cook – Educational Grant. Neptune Medical – Consultant. Olympus – Consultant. Steris – Consultant.
Neil Jariwalla, MD1, Joshua Kwon, MD1, Amirali Tavangar, MD1, Samuel Ji, MD1, David L. Cheung, MD2, Emily Bernale, BS1, Robert Lee, MD1, Jason Samarasena, MD1. P1853 - Comprehensive “One-Stop Shop” Esophageal Motility Workup During Propofol Endoscopy: Safe, Feasible, and Convenient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
