Monday Poster Session
Category: Esophagus
P1872 - Masks Are Gone but Dysphagia Remains
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- PP
Parth Patel, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Parth Patel, MD, Mokshad Gaonkar, , Mark Beasley, PhD, James Callaway, MD
University of Alabama at Birmingham, Birmingham, AL
Introduction: The SARS-CoV-2 virus(COVID-19) is a RNA virus that is transmitted via airborne droplets. COVID-19 typically presents with fever, cough, and congestion. In addition to the respiratory tract, the gastrointestinal(GI) and nervous systems may all be affected. Achalasia is a rare swallowing disorder in which there is loss of neurons in the esophagus which result in a loss of esophageal peristalsis and the failure of lower esophageal sphincter (LES) relaxation. The exact pathogenesis of achalasia is unknown but evidence suggests a degeneration of ganglion cells in the LES and esophageal body. In this case, we highlight a presentation of post-Covid achalasia, diagnostic studies, and treatment response.
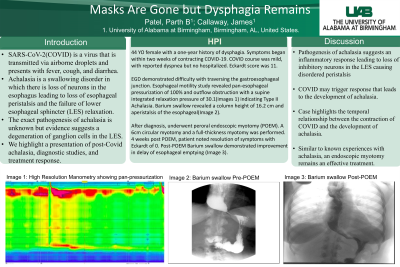
Case Description/Methods: A 44-year-old female present to GI clinic for a one year history of dysphagia and an accompanying 30lb weight loss. Notably, her symptoms began within two weeks of contracting COVID-19. She denied any dysphagia prior to this illness. Her COVID course was mild, with reported dyspnea but she was never hospitalized. Her Eckardt score at presentation was noted to be 11. Endoscopy demonstrated retained food and difficulty with traversing the gastro-esophageal junction. An esophageal motility study revealed failed peristalsis in all swallows, panesophageal pressurization, and outflow obstruction with a supine integrated relaxation pressure of 30.1. The study revealed Type II Achalasia. Barium swallow revealed column height at 5 minutes of 16.2 cm and aperistalsis of the esophageal. After diagnosis, she underwent peroral endoscopic myotomy (POEM). A progressive 6cm circular myotomy was performed in the distal esophagus(DE) and a full-thickness myotomy across the LES. 4 weeks post POEM the patient noted improvement in her symptoms. Her Eckardt score post POEM was 0.
Discussion: Current evidence of the pathogenesis of achalasia suggest an inflammatory response leading to selective loss of the inhibitory neurons in the DE and LES. This causes a clinical presentation of disordered peristalsis and failure of LES relaxation. Certain viruses, such as COVID-19, may trigger this response that leads to the development of achalasia. Although COVID-19 is known to cause GI disturbances, there have been few cases where it can contribute to the development of achalasia. Our case highlights the temporal relationship between the contraction of COVID-19 and the development of achalasia. Additionally, similar to known experiences with achalasia, an endoscopic myotomy remains an effective treatment.
Disclosures:
Parth Patel, MD, Mokshad Gaonkar, , Mark Beasley, PhD, James Callaway, MD. P1872 - Masks Are Gone but Dysphagia Remains, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Alabama at Birmingham, Birmingham, AL
Introduction: The SARS-CoV-2 virus(COVID-19) is a RNA virus that is transmitted via airborne droplets. COVID-19 typically presents with fever, cough, and congestion. In addition to the respiratory tract, the gastrointestinal(GI) and nervous systems may all be affected. Achalasia is a rare swallowing disorder in which there is loss of neurons in the esophagus which result in a loss of esophageal peristalsis and the failure of lower esophageal sphincter (LES) relaxation. The exact pathogenesis of achalasia is unknown but evidence suggests a degeneration of ganglion cells in the LES and esophageal body. In this case, we highlight a presentation of post-Covid achalasia, diagnostic studies, and treatment response.
Case Description/Methods: A 44-year-old female present to GI clinic for a one year history of dysphagia and an accompanying 30lb weight loss. Notably, her symptoms began within two weeks of contracting COVID-19. She denied any dysphagia prior to this illness. Her COVID course was mild, with reported dyspnea but she was never hospitalized. Her Eckardt score at presentation was noted to be 11. Endoscopy demonstrated retained food and difficulty with traversing the gastro-esophageal junction. An esophageal motility study revealed failed peristalsis in all swallows, panesophageal pressurization, and outflow obstruction with a supine integrated relaxation pressure of 30.1. The study revealed Type II Achalasia. Barium swallow revealed column height at 5 minutes of 16.2 cm and aperistalsis of the esophageal. After diagnosis, she underwent peroral endoscopic myotomy (POEM). A progressive 6cm circular myotomy was performed in the distal esophagus(DE) and a full-thickness myotomy across the LES. 4 weeks post POEM the patient noted improvement in her symptoms. Her Eckardt score post POEM was 0.
Discussion: Current evidence of the pathogenesis of achalasia suggest an inflammatory response leading to selective loss of the inhibitory neurons in the DE and LES. This causes a clinical presentation of disordered peristalsis and failure of LES relaxation. Certain viruses, such as COVID-19, may trigger this response that leads to the development of achalasia. Although COVID-19 is known to cause GI disturbances, there have been few cases where it can contribute to the development of achalasia. Our case highlights the temporal relationship between the contraction of COVID-19 and the development of achalasia. Additionally, similar to known experiences with achalasia, an endoscopic myotomy remains an effective treatment.
Disclosures:
Parth Patel indicated no relevant financial relationships.
Mokshad Gaonkar indicated no relevant financial relationships.
Mark Beasley indicated no relevant financial relationships.
James Callaway indicated no relevant financial relationships.
Parth Patel, MD, Mokshad Gaonkar, , Mark Beasley, PhD, James Callaway, MD. P1872 - Masks Are Gone but Dysphagia Remains, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
