Monday Poster Session
Category: Esophagus
P1880 - Lymphocytic Esophagitis: A Rare Cause of Dysphagia Presenting in an Elderly Patient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Hayden Rotramel, MD
Saint Louis University
St. Louis, MO
Presenting Author(s)
Hayden Rotramel, MD1, Mahmoud Y. Madi, MD2, Vinit V. Patil, MD1, Gregory S. Sayuk, MD3, Michael E. Presti, MD1, Jill E. Elwing, MD3
1Saint Louis University, St. Louis, MO; 2Saint Louis University Hospital, St. Louis, MO; 3Washington University in St. Louis, St. Louis, MO
Introduction: Lymphocytic esophagitis (LE) is a rare and poorly understood diagnosis. It is a subset of chronic esophagitis and is characterized by high numbers of intraepithelial lymphocytes located mainly around the peripapillary fields in the absence of intraepithelial granulocytes. The pathophysiology is unknown, but it most commonly effects middle-aged women. We present a rare case of LE in an elderly patient who initially presented with intermittent dysphagia.
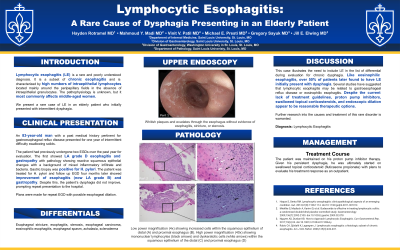
Case Description/Methods: An 83-year-old man with a history of gastroesophageal reflux disease presented for one year of intermittent difficulty swallowing solid foods and feeling that food was getting stuck in the mid-chest. The patient had undergone two esophagogastroduodenoscopies (EGDs) over the past year for evaluation. The first showed Los Angeles Classification (LA) grade D esophagitis and gastropathy. Microscopic evaluation of the esophageal brushing showed reactive squamous epithelial changes with a background of mixed inflammatory infiltrate and bacteria. Gastric biopsy was positive for H. pylori. He completed treatment for H. pylori infection and was continued on daily pantoprazole with adequate control of his acid reflux symptoms. Follow up EGD four months later showed improvement of esophagitis (now LA grade B) and gastropathy, however he continued to endorse dysphagia. He then underwent a third EGD with plans for empiric dilation. Endoscopy demonstrated whitish plaques and exudates through the esophagus and no evidence of esophagitis, stricture, or stenosis. Dilation was deferred and biopsies were taken from the esophagus and stomach. The gastric biopsy showed mild to moderate inflammation and was negative for H. pylori. Esophageal biopsies revealed moderate to severe lymphocytic infiltrate which was consistent with lymphocytosis pattern of injury. The patient was advised to continue his acid reducing medications and follow up in the gastroenterology clinic to discuss possible treatment with topical corticosteroids.
Discussion: This case illustrates the need to include LE in the list of differentials during evaluation of chronic dysphagia. Like eosinophilic esophagitis, over 50% of patients later found to have LE initially present with dysphagia. There are currently no guidelines for managing this diagnosis, however topical corticosteroids may prove beneficial as they have previously been effective in treating lymphocytic colitis. Further investigation into the causes and treatment of this rare disorder is warranted.

Disclosures:
Hayden Rotramel, MD1, Mahmoud Y. Madi, MD2, Vinit V. Patil, MD1, Gregory S. Sayuk, MD3, Michael E. Presti, MD1, Jill E. Elwing, MD3. P1880 - Lymphocytic Esophagitis: A Rare Cause of Dysphagia Presenting in an Elderly Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Louis University, St. Louis, MO; 2Saint Louis University Hospital, St. Louis, MO; 3Washington University in St. Louis, St. Louis, MO
Introduction: Lymphocytic esophagitis (LE) is a rare and poorly understood diagnosis. It is a subset of chronic esophagitis and is characterized by high numbers of intraepithelial lymphocytes located mainly around the peripapillary fields in the absence of intraepithelial granulocytes. The pathophysiology is unknown, but it most commonly effects middle-aged women. We present a rare case of LE in an elderly patient who initially presented with intermittent dysphagia.
Case Description/Methods: An 83-year-old man with a history of gastroesophageal reflux disease presented for one year of intermittent difficulty swallowing solid foods and feeling that food was getting stuck in the mid-chest. The patient had undergone two esophagogastroduodenoscopies (EGDs) over the past year for evaluation. The first showed Los Angeles Classification (LA) grade D esophagitis and gastropathy. Microscopic evaluation of the esophageal brushing showed reactive squamous epithelial changes with a background of mixed inflammatory infiltrate and bacteria. Gastric biopsy was positive for H. pylori. He completed treatment for H. pylori infection and was continued on daily pantoprazole with adequate control of his acid reflux symptoms. Follow up EGD four months later showed improvement of esophagitis (now LA grade B) and gastropathy, however he continued to endorse dysphagia. He then underwent a third EGD with plans for empiric dilation. Endoscopy demonstrated whitish plaques and exudates through the esophagus and no evidence of esophagitis, stricture, or stenosis. Dilation was deferred and biopsies were taken from the esophagus and stomach. The gastric biopsy showed mild to moderate inflammation and was negative for H. pylori. Esophageal biopsies revealed moderate to severe lymphocytic infiltrate which was consistent with lymphocytosis pattern of injury. The patient was advised to continue his acid reducing medications and follow up in the gastroenterology clinic to discuss possible treatment with topical corticosteroids.
Discussion: This case illustrates the need to include LE in the list of differentials during evaluation of chronic dysphagia. Like eosinophilic esophagitis, over 50% of patients later found to have LE initially present with dysphagia. There are currently no guidelines for managing this diagnosis, however topical corticosteroids may prove beneficial as they have previously been effective in treating lymphocytic colitis. Further investigation into the causes and treatment of this rare disorder is warranted.

Figure: Figure: Part 1 is an endoscopic view showing whitish plaques and exudates through the esophagus and no evidence of esophagitis, stricture, or stenosis. Part 2 shows Increased lymphocytes in the distal and proximal esophagus. Low power magnification (4x) shows increased cells within the squamous epithelium of distal (A) and proximal esophagus (B). The high power magnification (40x) of the inset show's mononuclear lymphocytes (black arrows) and dyskeratotic cells (white arrows) within the squamous epithelium of the distal (C) and proximal esophagus (D).
Disclosures:
Hayden Rotramel indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Vinit Patil indicated no relevant financial relationships.
Gregory Sayuk indicated no relevant financial relationships.
Michael Presti indicated no relevant financial relationships.
Jill Elwing indicated no relevant financial relationships.
Hayden Rotramel, MD1, Mahmoud Y. Madi, MD2, Vinit V. Patil, MD1, Gregory S. Sayuk, MD3, Michael E. Presti, MD1, Jill E. Elwing, MD3. P1880 - Lymphocytic Esophagitis: A Rare Cause of Dysphagia Presenting in an Elderly Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
