Monday Poster Session
Category: Esophagus
P1882 - An Interesting Case of Necrotic "Black" Esophagus
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ayham Khrais, DO
Rutgers New Jersey Medical School
Newark, New Jersey
Presenting Author(s)
Ayham Khrais, DO, Hareem Rehman, MD, Arthi Palani, MD, Luisa De Souza, MD, Param Patel, MD
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Acute esophageal necrosis (AEN), AKA “black esophagus,” denotes proximally extending circumferential mucosal damage of the distal esophagus, giving it a blackened appearance. Causes include ischemia or direct chemical mucosal injury. Patients often present with signs of upper gastrointestinal bleeding (UGIB). AEN is rare, with incidence ranging from 0.01% to 0.28%. Management includes intravenous fluid resuscitation, cessation of oral intake, and intravenous proton pump inhibitor therapy. Here, we describe an interesting case of AEN likely brought on by a combination of septic shock and subsequent vasopressor therapy resulting in esophageal mucosal ischemia.
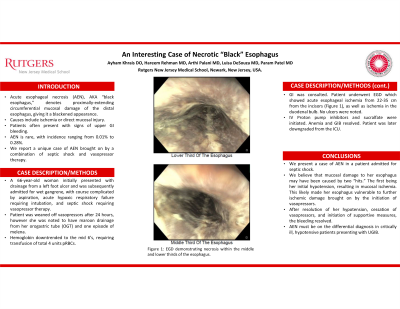
Case Description/Methods: A 66-year-old woman with a history of peripheral artery disease, ischemic stroke, and coronary artery disease who initially presented with drainage from a left foot ulcer, found to have wet gangrene for which she was treated with broad spectrum antibiotics. She developed hypoxic respiratory failure secondary to aspiration, and septic shock, with systolic blood pressure in the 80s. She was intubated, started on norepinephrine and upgraded to ICU. Antibiotics were escalated. She was weaned off vasopressors after 24 hours. Prior to cessation of vasopressors, she had maroon drainage from her orogastric tube, and one episode of melena. Hemoglobin was downtrending with a nadir of 6.2, requiring 2 units of pRBCs. Gastroenterology was consulted and endoscopy was performed, demonstrating acute esophageal ischemia located 22-35 cm from the incisors, as well as ischemia in the duodenum. After resolution of the septic shock and continued hemodynamic support with IV fluids and PPI, patient’s anemia and bleeding improved.
Discussion: Here, we present a case of AEN in a patient admitted for septic shock. We believe that mucosal damage to her esophagus may have been caused by two “hits.” The first hit being her initial hypotension, resulting in mucosal ischemia. This likely made her vulnerable to further ischemic damage brought on by initiation of vasopressors. After resolution of her hypotension, cessation of vasopressors, and initiation of supportive measures, the bleeding resolved. AEN must be on the differential in critically ill, hypotensive patients presenting with UGIB.

Disclosures:
Ayham Khrais, DO, Hareem Rehman, MD, Arthi Palani, MD, Luisa De Souza, MD, Param Patel, MD. P1882 - An Interesting Case of Necrotic "Black" Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Acute esophageal necrosis (AEN), AKA “black esophagus,” denotes proximally extending circumferential mucosal damage of the distal esophagus, giving it a blackened appearance. Causes include ischemia or direct chemical mucosal injury. Patients often present with signs of upper gastrointestinal bleeding (UGIB). AEN is rare, with incidence ranging from 0.01% to 0.28%. Management includes intravenous fluid resuscitation, cessation of oral intake, and intravenous proton pump inhibitor therapy. Here, we describe an interesting case of AEN likely brought on by a combination of septic shock and subsequent vasopressor therapy resulting in esophageal mucosal ischemia.
Case Description/Methods: A 66-year-old woman with a history of peripheral artery disease, ischemic stroke, and coronary artery disease who initially presented with drainage from a left foot ulcer, found to have wet gangrene for which she was treated with broad spectrum antibiotics. She developed hypoxic respiratory failure secondary to aspiration, and septic shock, with systolic blood pressure in the 80s. She was intubated, started on norepinephrine and upgraded to ICU. Antibiotics were escalated. She was weaned off vasopressors after 24 hours. Prior to cessation of vasopressors, she had maroon drainage from her orogastric tube, and one episode of melena. Hemoglobin was downtrending with a nadir of 6.2, requiring 2 units of pRBCs. Gastroenterology was consulted and endoscopy was performed, demonstrating acute esophageal ischemia located 22-35 cm from the incisors, as well as ischemia in the duodenum. After resolution of the septic shock and continued hemodynamic support with IV fluids and PPI, patient’s anemia and bleeding improved.
Discussion: Here, we present a case of AEN in a patient admitted for septic shock. We believe that mucosal damage to her esophagus may have been caused by two “hits.” The first hit being her initial hypotension, resulting in mucosal ischemia. This likely made her vulnerable to further ischemic damage brought on by initiation of vasopressors. After resolution of her hypotension, cessation of vasopressors, and initiation of supportive measures, the bleeding resolved. AEN must be on the differential in critically ill, hypotensive patients presenting with UGIB.

Figure: Figure 1: EGD demonstrating necrosis within the middle third of the esophagus.
EGD: esophagogastroduodeonscopy.
EGD: esophagogastroduodeonscopy.
Disclosures:
Ayham Khrais indicated no relevant financial relationships.
Hareem Rehman indicated no relevant financial relationships.
Arthi Palani indicated no relevant financial relationships.
Luisa De Souza indicated no relevant financial relationships.
Param Patel indicated no relevant financial relationships.
Ayham Khrais, DO, Hareem Rehman, MD, Arthi Palani, MD, Luisa De Souza, MD, Param Patel, MD. P1882 - An Interesting Case of Necrotic "Black" Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
