Monday Poster Session
Category: Esophagus
P1885 - A Very Late Complication of Laparoscopic Heller Myotomy: After 30 Years, Blown out Myotomy Results in Esophagectomy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Robert Spiller, DO, MS
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Jacob Cravens, MD1, Robert Spiller, DO, MS2, John McCarthy, MD2
1Bassett Army Community Hospital, Fort Wainright, AK; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Persistent symptoms of achalasia occur in 10-20% of patients that undergo laparoscopic Heller myotomy (LHM) or per oral endoscopic myotomy (POEM). A mimicker of achalasia in post-myotomy patients is a blown-out myotomy (BOM) wherein a pseudodiverticulum develops in the distal esophagus at the site of prior myotomy. Studies report a 17.8% prevalence of BOM after myotomy, 74% occurring post-LHM and 26% post-POEM. We review a case of late development of BOM after LHM and esophagectomy as treatment.
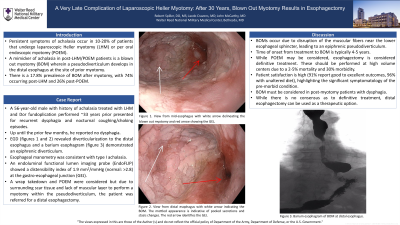
Case Description/Methods: A 56-year-old male with history of achalasia treated with LHM and fundoplication performed ~33 years ago presented for recurrent dysphagia. Up until the prior few months, the patient reported no dysphagia since his myotomy. He reported nocturnal coughing and vomiting occurring hours after consuming solid meals. He underwent an EGD (figure 1a) which revealed diverticularization to the distal esophagus with an intact surgical wrap. Cross-sectional imaging ruled out malignancy. A barium esophagram (figure 1b) demonstrated a diverticulum adjacent to the gastroesophageal junction (GEJ). Esophageal manometry was consistent with type I achalasia. An endoluminal functional lumen imaging probe (EndoFLIP) showed a distensibility index of 1.9 mm2/mmHg (normal: >2.8) at the GEJ. The lower esophageal sphincter (LES) was easily traversed with a standard endoscope without resistance and balloon dilation at LES resulted in no dilation effect. A wrap takedown and POEM were considered but due to surrounding scar tissue and lack of muscular layer to perform a myotomy within the pseudodiverticulum, the patient underwent a distal esophagectomy with resolution of his presenting symptoms.
Discussion: This case illustrates the very late development of BOM after LHM and subsequent treatment via esophagectomy. BOMs occur due to disruption of the muscular fibers near the LES, leading to an epiphrenic pseudodiverticulum. While POEM may be considered, esophagectomy is considered definitive treatment. These cases should be performed at high-volume centers due to a 2-5% mortality and 30% morbidity. However, patient satisfaction is high (91% report good to excellent outcomes, 96% with unaltered diet), highlighting the significant symptomatology of the pre-morbid condition. This case demonstrates that BOM must be considered in post-myotomy patients who have recurrent dysphagia. It also outlines a diagnostic evaluation for this entity and suggests that distal esophagectomy can be used as a therapeutic option.

Disclosures:
Jacob Cravens, MD1, Robert Spiller, DO, MS2, John McCarthy, MD2. P1885 - A Very Late Complication of Laparoscopic Heller Myotomy: After 30 Years, Blown out Myotomy Results in Esophagectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Bassett Army Community Hospital, Fort Wainright, AK; 2Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Persistent symptoms of achalasia occur in 10-20% of patients that undergo laparoscopic Heller myotomy (LHM) or per oral endoscopic myotomy (POEM). A mimicker of achalasia in post-myotomy patients is a blown-out myotomy (BOM) wherein a pseudodiverticulum develops in the distal esophagus at the site of prior myotomy. Studies report a 17.8% prevalence of BOM after myotomy, 74% occurring post-LHM and 26% post-POEM. We review a case of late development of BOM after LHM and esophagectomy as treatment.
Case Description/Methods: A 56-year-old male with history of achalasia treated with LHM and fundoplication performed ~33 years ago presented for recurrent dysphagia. Up until the prior few months, the patient reported no dysphagia since his myotomy. He reported nocturnal coughing and vomiting occurring hours after consuming solid meals. He underwent an EGD (figure 1a) which revealed diverticularization to the distal esophagus with an intact surgical wrap. Cross-sectional imaging ruled out malignancy. A barium esophagram (figure 1b) demonstrated a diverticulum adjacent to the gastroesophageal junction (GEJ). Esophageal manometry was consistent with type I achalasia. An endoluminal functional lumen imaging probe (EndoFLIP) showed a distensibility index of 1.9 mm2/mmHg (normal: >2.8) at the GEJ. The lower esophageal sphincter (LES) was easily traversed with a standard endoscope without resistance and balloon dilation at LES resulted in no dilation effect. A wrap takedown and POEM were considered but due to surrounding scar tissue and lack of muscular layer to perform a myotomy within the pseudodiverticulum, the patient underwent a distal esophagectomy with resolution of his presenting symptoms.
Discussion: This case illustrates the very late development of BOM after LHM and subsequent treatment via esophagectomy. BOMs occur due to disruption of the muscular fibers near the LES, leading to an epiphrenic pseudodiverticulum. While POEM may be considered, esophagectomy is considered definitive treatment. These cases should be performed at high-volume centers due to a 2-5% mortality and 30% morbidity. However, patient satisfaction is high (91% report good to excellent outcomes, 96% with unaltered diet), highlighting the significant symptomatology of the pre-morbid condition. This case demonstrates that BOM must be considered in post-myotomy patients who have recurrent dysphagia. It also outlines a diagnostic evaluation for this entity and suggests that distal esophagectomy can be used as a therapeutic option.

Figure: View of distal esophagus with white arrow delineating the BOM and red arrow showing the GEJ (Figure 1A). Barium esophagram noting the diverticularization and BOM at the distal esophagus (Figure 1B).
Disclosures:
Jacob Cravens indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
John McCarthy indicated no relevant financial relationships.
Jacob Cravens, MD1, Robert Spiller, DO, MS2, John McCarthy, MD2. P1885 - A Very Late Complication of Laparoscopic Heller Myotomy: After 30 Years, Blown out Myotomy Results in Esophagectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
