Monday Poster Session
Category: Esophagus
P1892 - A Case of Primary Malignant Melanoma of the Esophagus
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Usman S. Ansari, DO
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Usman S. Ansari, DO, Ziad El-Zaatari, MD, Mary Schwartz, MD, Rachel Schiesser, MD
Houston Methodist Hospital, Houston, TX
Introduction: Primary malignant melanoma of the esophagus (PMME) is an extremely rare cancer that makes up 0.1-0.8% of all oro-esophageal cancers and < 0.05% of all melanoma subtypes, with only approximately 350 cases reported in the literature since 1906. It is known to be a highly aggressive tumor with a poor prognosis, and there is no standardized treatment. Recently the use of programmed cell death protein 1 (PD-1) inhibitors has been shown to extend the survival of patients with unresectable or metastatic PMME. Here we present a rare case of PMME treated with immunotherapy with a favorable response.
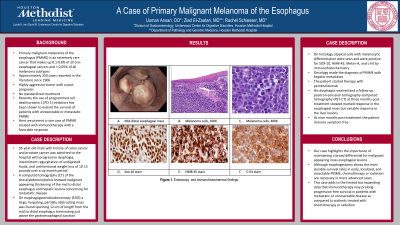
Case Description/Methods: 95-year-old male with history of colon cancer and prostate cancer was admitted to the hospital with progressive dysphagia, intermittent regurgitation of undigested foods, and unintentional weight loss of 10-15 pounds over a six-month period. A computed tomography (CT) of the chest/abdomen/pelvis showed malignant appearing thickening of the mid to distal esophagus and hepatic lesions concerning for metastatic disease. On esophagogastroduodenoscopy (EGD) a large, fungating, partially obstructing mass was found spanning 12-cm of length from the mid to distal esophagus terminating just above the gastroesophageal junction. On histology atypical cells with melanocytic differentiation were seen and were positive for SOX-10, HMB-45, Melan-A, and c-kit by immunohistochemistry. Oncology made the diagnosis of PMME with hepatic metastases. The patient started therapy with pembrolizumab. His dysphagia resolved and a follow-up positron emission tomography-computed tomography (PET-CT) at three months post-treatment showed marked response in the esophageal mass but variable response in the liver lesions. At nine months post-treatment the patient remains symptom free.
Discussion: Our case highlights the importance of maintaining a broad differential for malignant appearing mass esophageal lesions. Although esophagectomy shows the most durable survival rates in early, localized, and resectable PMME, chemotherapy or radiation are necessary in more advanced cases. This case adds to the limited but expanding data that immunotherapy may prolong progression free survival in patients with metastatic or unresectable disease as compared to patients treated with chemotherapy or radiation.

Disclosures:
Usman S. Ansari, DO, Ziad El-Zaatari, MD, Mary Schwartz, MD, Rachel Schiesser, MD. P1892 - A Case of Primary Malignant Melanoma of the Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Houston Methodist Hospital, Houston, TX
Introduction: Primary malignant melanoma of the esophagus (PMME) is an extremely rare cancer that makes up 0.1-0.8% of all oro-esophageal cancers and < 0.05% of all melanoma subtypes, with only approximately 350 cases reported in the literature since 1906. It is known to be a highly aggressive tumor with a poor prognosis, and there is no standardized treatment. Recently the use of programmed cell death protein 1 (PD-1) inhibitors has been shown to extend the survival of patients with unresectable or metastatic PMME. Here we present a rare case of PMME treated with immunotherapy with a favorable response.
Case Description/Methods: 95-year-old male with history of colon cancer and prostate cancer was admitted to the hospital with progressive dysphagia, intermittent regurgitation of undigested foods, and unintentional weight loss of 10-15 pounds over a six-month period. A computed tomography (CT) of the chest/abdomen/pelvis showed malignant appearing thickening of the mid to distal esophagus and hepatic lesions concerning for metastatic disease. On esophagogastroduodenoscopy (EGD) a large, fungating, partially obstructing mass was found spanning 12-cm of length from the mid to distal esophagus terminating just above the gastroesophageal junction. On histology atypical cells with melanocytic differentiation were seen and were positive for SOX-10, HMB-45, Melan-A, and c-kit by immunohistochemistry. Oncology made the diagnosis of PMME with hepatic metastases. The patient started therapy with pembrolizumab. His dysphagia resolved and a follow-up positron emission tomography-computed tomography (PET-CT) at three months post-treatment showed marked response in the esophageal mass but variable response in the liver lesions. At nine months post-treatment the patient remains symptom free.
Discussion: Our case highlights the importance of maintaining a broad differential for malignant appearing mass esophageal lesions. Although esophagectomy shows the most durable survival rates in early, localized, and resectable PMME, chemotherapy or radiation are necessary in more advanced cases. This case adds to the limited but expanding data that immunotherapy may prolong progression free survival in patients with metastatic or unresectable disease as compared to patients treated with chemotherapy or radiation.

Figure: PMME endoscopic view, histology, and immunohistochemical stains
Disclosures:
Usman Ansari indicated no relevant financial relationships.
Ziad El-Zaatari indicated no relevant financial relationships.
Mary Schwartz indicated no relevant financial relationships.
Rachel Schiesser indicated no relevant financial relationships.
Usman S. Ansari, DO, Ziad El-Zaatari, MD, Mary Schwartz, MD, Rachel Schiesser, MD. P1892 - A Case of Primary Malignant Melanoma of the Esophagus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

