Monday Poster Session
Category: Esophagus
P1915 - Esophageal Parakeratosis - A Benign Mimic of Malignant Esophageal Lesions
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Justice Arhinful, MD
Howard University Hospital
Washington, DC
Presenting Author(s)
Justice Arhinful, MD, Abdullahi Musa, MD, Philip Oppong-Twene, MD, MPH, Chineduu Okeke, MD, Babak Shokrani, MD, Farshad Aduli, MD
Howard University Hospital, Washington, DC
Introduction: Several benign esophageal lesions may be encountered during esophagogastroduodenoscopy (EGD). Although these lesions are mostly asymptomatic and do not usually have malignant transformation potential, they may nonetheless pose diagnostic and management conundrum to clinicians. One of such lesions is esophageal parakeratosis as it can mimic other conditions such as superficial esophageal neoplasm. Esophageal parakeratosis is rare and its endoscopic appearance and clinical significance have not been well described. We present a case of esophageal parakeratosis with concurrent esophagitis resembling superficial esophageal neoplasm endoscopically.
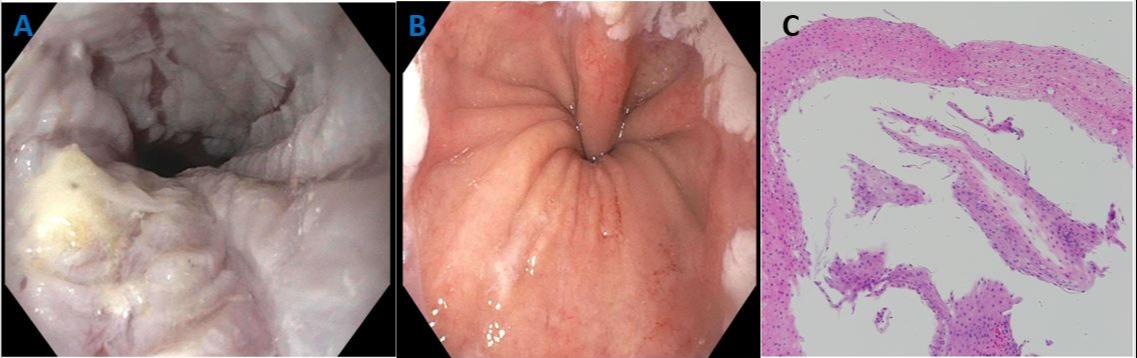
Case Description/Methods: A 67-year-old African American female with history of chronic pancreatitis, hypertension, GERD, and asthma presented to the GI clinic with an 8/10 stabbing epigastric pain, radiating to the back. Pain usually lasts 2-3 hours and it is aggravated by meals and unresponsive to low dose pantoprazole. She denied fever, cough, chest pain, diarrhea, melena, hematochezia. EGD showed thickened whitish sloughed membranous mucosa with finger-like projections involving the middle and distal third of esophagus along with LA grade C esophagitis (Images A & B), antral gastritis and 2 non-bleeding superficial antral ulcers. Several biopsies taken from the middle and distal esophagus were reported as consistent with esophageal parakeratosis (Image C) with concurrent esophagitis without evidence of fungal infection. PPI dose was maximized with resultant resolution of her symptoms.
Discussion: Esophageal parakeratosis is an uncommon endoscopic finding of unknown significance, although it has been reported to be associated with alcoholic cirrhosis, tylosis, zinc deficiency, and squamous cell carcinomas of the esophagus and, head and neck. Histologically, it is described as epithelial acanthosis, basal hyperplasia, and a dense compact layer of parakeratosis, usually featuring cytoplasmic eosinophilia and pyknotic nuclei, covered by an outer layer of nonnucleated squamous cells. However, given its endoscopic appearance as whitish, membranous, linear plaques, it can easily be misdiagnosed as candida esophagitis, eosinophilic esophagitis and neoplastic lesions such as squamous cell carcinoma. In the clinical setting, clinicians must be aware of the above associations, especially, squamous cell carcinoma, such that a careful evaluation of the esophagus and head and neck region for cancer should be done at the time of diagnosis of esophageal parakeratosis.
Disclosures:
Justice Arhinful, MD, Abdullahi Musa, MD, Philip Oppong-Twene, MD, MPH, Chineduu Okeke, MD, Babak Shokrani, MD, Farshad Aduli, MD. P1915 - Esophageal Parakeratosis - A Benign Mimic of Malignant Esophageal Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Howard University Hospital, Washington, DC
Introduction: Several benign esophageal lesions may be encountered during esophagogastroduodenoscopy (EGD). Although these lesions are mostly asymptomatic and do not usually have malignant transformation potential, they may nonetheless pose diagnostic and management conundrum to clinicians. One of such lesions is esophageal parakeratosis as it can mimic other conditions such as superficial esophageal neoplasm. Esophageal parakeratosis is rare and its endoscopic appearance and clinical significance have not been well described. We present a case of esophageal parakeratosis with concurrent esophagitis resembling superficial esophageal neoplasm endoscopically.
Case Description/Methods: A 67-year-old African American female with history of chronic pancreatitis, hypertension, GERD, and asthma presented to the GI clinic with an 8/10 stabbing epigastric pain, radiating to the back. Pain usually lasts 2-3 hours and it is aggravated by meals and unresponsive to low dose pantoprazole. She denied fever, cough, chest pain, diarrhea, melena, hematochezia. EGD showed thickened whitish sloughed membranous mucosa with finger-like projections involving the middle and distal third of esophagus along with LA grade C esophagitis (Images A & B), antral gastritis and 2 non-bleeding superficial antral ulcers. Several biopsies taken from the middle and distal esophagus were reported as consistent with esophageal parakeratosis (Image C) with concurrent esophagitis without evidence of fungal infection. PPI dose was maximized with resultant resolution of her symptoms.
Discussion: Esophageal parakeratosis is an uncommon endoscopic finding of unknown significance, although it has been reported to be associated with alcoholic cirrhosis, tylosis, zinc deficiency, and squamous cell carcinomas of the esophagus and, head and neck. Histologically, it is described as epithelial acanthosis, basal hyperplasia, and a dense compact layer of parakeratosis, usually featuring cytoplasmic eosinophilia and pyknotic nuclei, covered by an outer layer of nonnucleated squamous cells. However, given its endoscopic appearance as whitish, membranous, linear plaques, it can easily be misdiagnosed as candida esophagitis, eosinophilic esophagitis and neoplastic lesions such as squamous cell carcinoma. In the clinical setting, clinicians must be aware of the above associations, especially, squamous cell carcinoma, such that a careful evaluation of the esophagus and head and neck region for cancer should be done at the time of diagnosis of esophageal parakeratosis.
Figure: Image A: Endoscopic phtograph showing whitish sloughed membranous thickened mucosa with finger-like projections.
Image B: Endoscopic photograph showing LA grade C esophagitis.
Image C: Medium power magnification depicting sloughed off squamous mucosa with parakeratosis
Image B: Endoscopic photograph showing LA grade C esophagitis.
Image C: Medium power magnification depicting sloughed off squamous mucosa with parakeratosis
Disclosures:
Justice Arhinful indicated no relevant financial relationships.
Abdullahi Musa indicated no relevant financial relationships.
Philip Oppong-Twene indicated no relevant financial relationships.
Chineduu Okeke indicated no relevant financial relationships.
Babak Shokrani indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Justice Arhinful, MD, Abdullahi Musa, MD, Philip Oppong-Twene, MD, MPH, Chineduu Okeke, MD, Babak Shokrani, MD, Farshad Aduli, MD. P1915 - Esophageal Parakeratosis - A Benign Mimic of Malignant Esophageal Lesions, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
