Monday Poster Session
Category: Esophagus
P1919 - A Rare Case of Kleine-Levin Syndrome Exacerbated by Erosive Esophagitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- TR
Tabeer Rana, DO
Allegheny Health Network
Pittsburgh, PA
Presenting Author(s)
Samuel Purkey, DO, Tabeer Rana, DO, Aaisha Shah, MD, Marisa Isaacson, MD
Allegheny Health Network, Pittsburgh, PA
Introduction: Kleine-Levin Syndrome (KLS) is a syndrome associated with intermittent hypersomnolence, behavioral and cognitive disturbances, hyperphagia, and hypersexuality. No definitive cause of KLS has been determined. While the gut-brain connection is well established, we present an atypical presentation of a relapsing episode of KLS due to untreated severe esophagitis.
Case Description/Methods: We present a 37-year-old male with history of KLS presenting to the hospital for encephalopathy and concern for KLS relapse. Symptoms included confusion, inability to concentrate, dysphoria, pressured speech, and hyperphagia. He had three hospitalizations in three months that psychiatry theorized was a prolonged relapse of KLS despite treatment.
On presentation, he was hemodynamically stable and labs were unremarkable. Alcohol and toxin screen were negative. Exam noted dysphoric mood, agitation, and catatonia. Psychiatry initiated treatment with lorazepam and haloperidol. Later, he reported chest, throat, abdomen pain. Repeat labs revealed a leukocytosis and a computed tomographic chest and abdomen with contrast noted severe distal esophageal inflammation. He was started on pantoprazole and GI was consulted.
He underwent an EGD revealing severe Las Angeles (LA) grade D erosive esophagitis in distal esophagus and LA grade B esophagitis in proximal esophagus without gastric or duodenal abnormalities. Biopsies revealed distal fibrinopurulent exudate consistent with an ulcer and proximal inflammatory changes consistent with reflux. His mental status improved significantly while on pantoprazole and sucralfate. His mental clarity was consistent with his baseline.
Psychiatry theorized his protracted KLS episode was due to esophagitis and associated inflammatory response. He was discharged home with a lorazepam taper down to a maintenance dose and pantoprazole twice daily. He was scheduled for repeat EGD in 12 weeks.
Discussion: We present an atypical case of KLS exacerbation refractory to benzodiazepines due to underlying inflammation from esophagitis. Although not common, it is important to keep our differentials broad when it comes to neuropsychiatric disorders with exacerbation and the gut-brain connection. In atypical psychiatry presentations, optimizing other medical conditions, such as esophagitis, remains important, as they can contribute to exacerbations and refractory disease. The patient’s KLS was refractory to standard treatment. Upon treatment of esophagitis, the patient’s mental status returned to baseline.

Disclosures:
Samuel Purkey, DO, Tabeer Rana, DO, Aaisha Shah, MD, Marisa Isaacson, MD. P1919 - A Rare Case of Kleine-Levin Syndrome Exacerbated by Erosive Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Allegheny Health Network, Pittsburgh, PA
Introduction: Kleine-Levin Syndrome (KLS) is a syndrome associated with intermittent hypersomnolence, behavioral and cognitive disturbances, hyperphagia, and hypersexuality. No definitive cause of KLS has been determined. While the gut-brain connection is well established, we present an atypical presentation of a relapsing episode of KLS due to untreated severe esophagitis.
Case Description/Methods: We present a 37-year-old male with history of KLS presenting to the hospital for encephalopathy and concern for KLS relapse. Symptoms included confusion, inability to concentrate, dysphoria, pressured speech, and hyperphagia. He had three hospitalizations in three months that psychiatry theorized was a prolonged relapse of KLS despite treatment.
On presentation, he was hemodynamically stable and labs were unremarkable. Alcohol and toxin screen were negative. Exam noted dysphoric mood, agitation, and catatonia. Psychiatry initiated treatment with lorazepam and haloperidol. Later, he reported chest, throat, abdomen pain. Repeat labs revealed a leukocytosis and a computed tomographic chest and abdomen with contrast noted severe distal esophageal inflammation. He was started on pantoprazole and GI was consulted.
He underwent an EGD revealing severe Las Angeles (LA) grade D erosive esophagitis in distal esophagus and LA grade B esophagitis in proximal esophagus without gastric or duodenal abnormalities. Biopsies revealed distal fibrinopurulent exudate consistent with an ulcer and proximal inflammatory changes consistent with reflux. His mental status improved significantly while on pantoprazole and sucralfate. His mental clarity was consistent with his baseline.
Psychiatry theorized his protracted KLS episode was due to esophagitis and associated inflammatory response. He was discharged home with a lorazepam taper down to a maintenance dose and pantoprazole twice daily. He was scheduled for repeat EGD in 12 weeks.
Discussion: We present an atypical case of KLS exacerbation refractory to benzodiazepines due to underlying inflammation from esophagitis. Although not common, it is important to keep our differentials broad when it comes to neuropsychiatric disorders with exacerbation and the gut-brain connection. In atypical psychiatry presentations, optimizing other medical conditions, such as esophagitis, remains important, as they can contribute to exacerbations and refractory disease. The patient’s KLS was refractory to standard treatment. Upon treatment of esophagitis, the patient’s mental status returned to baseline.

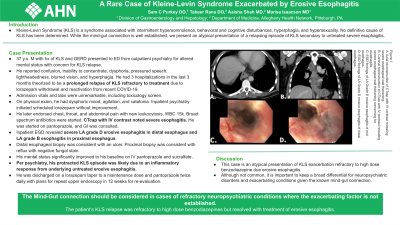
Figure: A: Axial reconstruction of the CT chest and abdomen with IV contrast revealing severe esophageal wall thickening.
B: Coronal reconstruction of the CT chest and abdomen with IV contrast revealing severe esophageal wall thickening concerning for esophagitis.
C: EGD findings of LA Grade D erosive esophagitis of the mid esophagus.
D: EGD findings of LA Grade D erosive esophagitis of the distal esophagus.
B: Coronal reconstruction of the CT chest and abdomen with IV contrast revealing severe esophageal wall thickening concerning for esophagitis.
C: EGD findings of LA Grade D erosive esophagitis of the mid esophagus.
D: EGD findings of LA Grade D erosive esophagitis of the distal esophagus.
Disclosures:
Samuel Purkey indicated no relevant financial relationships.
Tabeer Rana indicated no relevant financial relationships.
Aaisha Shah indicated no relevant financial relationships.
Marisa Isaacson indicated no relevant financial relationships.
Samuel Purkey, DO, Tabeer Rana, DO, Aaisha Shah, MD, Marisa Isaacson, MD. P1919 - A Rare Case of Kleine-Levin Syndrome Exacerbated by Erosive Esophagitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
