Monday Poster Session
Category: Esophagus
P1925 - The Black Esophagus: A Case of Acute Esophageal Necrosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- BZ
Boris Zhong, DO
Baylor Scott & White
Temple, TX
Presenting Author(s)
Boris Zhong, DO1, Mark Shell, DO1, Mark Jeffries, DO2, Mauricio Jones, DO1
1Baylor Scott & White, Temple, TX; 2Baylor Scott & White Health, Temple, TX
Introduction: Acute esophageal necrosis, also known as necrotizing esophagitis or “black esophagus”, is a rare endoscopic finding characterized by circumferential, black discoloration of the distal esophagus with sharp transition at the gastroesophageal junction. Its etiology is multifactorial and carries a poor prognosis as a reflection of the severity of underlying medical conditions. We present a case of AEN in an ESRD patient with urosepsis.
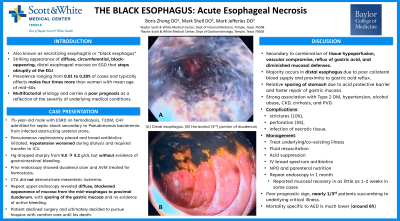
Case Description/Methods: A 75-year-old male with ESRD on hemodialysis, diabetes mellitus, chronic heart failure was admitted for septic shock secondary to Pseudomonas bacteremia from infected obstructing ureteral stone. Percutaneous nephrostomy was placed and broad antibiotics initiated. Hypotension worsened during dialysis and required transfer to ICU for vasopressor support. The following day, his hemoglobin dropped sharply from 9.5 to 5.2 g/dL but without evidence of gastrointestinal bleeding though nausea and vomiting. Prior endoscopy showed duodenal ulcer and AVM treated for hemostasis. Repeat upper endoscopy revealed diffuse, blackened appearance of mucosa from the mid-esophagus to proximal duodenum, with sparing of the gastric mucosa and no evidence of active bleeding. CTA did not demonstrate mesenteric ischemia. Potential surgery offered which patient declined and ultimately decided to pursue hospice with comfort care until his death.
Discussion: Acute esophageal necrosis is an uncommon process with a striking appearance that almost universally affects the distal esophagus and abruptly stops at the GEJ. Its etiology is multifactorial from a combination of tissue hypoperfusion, reflux of gastric acid, and diminished mucosal defenses1. Reported prevalence has ranged from 0.01 to 0.28% of cases and typically affects males four times more than women with mean age of mid-60s2,3. Strong association is seen in patients with hypoalbuminemia, anemia, renal insufficiency, hyperglycemia, and in low-flow state. Up to 32% mortality has been reported which is largely related to severity of underlying disease, as death directly attributable to AEN is much lower at 6%1,4. Our septic patient requiring dialysis fit the classic presentation of someone susceptible to AEN which was incidentally seen on EGD, though without evidence of bleeding. Our patient ultimately succumbed to his underlying disease. However, proper management with resuscitation, acid suppression, antibiotics, and parenteral nutrition have shown favorable outcome in more than 60% of patients.

Disclosures:
Boris Zhong, DO1, Mark Shell, DO1, Mark Jeffries, DO2, Mauricio Jones, DO1. P1925 - The Black Esophagus: A Case of Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baylor Scott & White, Temple, TX; 2Baylor Scott & White Health, Temple, TX
Introduction: Acute esophageal necrosis, also known as necrotizing esophagitis or “black esophagus”, is a rare endoscopic finding characterized by circumferential, black discoloration of the distal esophagus with sharp transition at the gastroesophageal junction. Its etiology is multifactorial and carries a poor prognosis as a reflection of the severity of underlying medical conditions. We present a case of AEN in an ESRD patient with urosepsis.
Case Description/Methods: A 75-year-old male with ESRD on hemodialysis, diabetes mellitus, chronic heart failure was admitted for septic shock secondary to Pseudomonas bacteremia from infected obstructing ureteral stone. Percutaneous nephrostomy was placed and broad antibiotics initiated. Hypotension worsened during dialysis and required transfer to ICU for vasopressor support. The following day, his hemoglobin dropped sharply from 9.5 to 5.2 g/dL but without evidence of gastrointestinal bleeding though nausea and vomiting. Prior endoscopy showed duodenal ulcer and AVM treated for hemostasis. Repeat upper endoscopy revealed diffuse, blackened appearance of mucosa from the mid-esophagus to proximal duodenum, with sparing of the gastric mucosa and no evidence of active bleeding. CTA did not demonstrate mesenteric ischemia. Potential surgery offered which patient declined and ultimately decided to pursue hospice with comfort care until his death.
Discussion: Acute esophageal necrosis is an uncommon process with a striking appearance that almost universally affects the distal esophagus and abruptly stops at the GEJ. Its etiology is multifactorial from a combination of tissue hypoperfusion, reflux of gastric acid, and diminished mucosal defenses1. Reported prevalence has ranged from 0.01 to 0.28% of cases and typically affects males four times more than women with mean age of mid-60s2,3. Strong association is seen in patients with hypoalbuminemia, anemia, renal insufficiency, hyperglycemia, and in low-flow state. Up to 32% mortality has been reported which is largely related to severity of underlying disease, as death directly attributable to AEN is much lower at 6%1,4. Our septic patient requiring dialysis fit the classic presentation of someone susceptible to AEN which was incidentally seen on EGD, though without evidence of bleeding. Our patient ultimately succumbed to his underlying disease. However, proper management with resuscitation, acid suppression, antibiotics, and parenteral nutrition have shown favorable outcome in more than 60% of patients.

Figure: Endoscopy visualization of mid esophagus (A), distal esophagus (B), duodenal bulb (C), horizontal (3rd) portion of duodenum (D) showing diffuse, circumferential, black appearance of the mucosa.
Disclosures:
Boris Zhong indicated no relevant financial relationships.
Mark Shell indicated no relevant financial relationships.
Mark Jeffries indicated no relevant financial relationships.
Mauricio Jones indicated no relevant financial relationships.
Boris Zhong, DO1, Mark Shell, DO1, Mark Jeffries, DO2, Mauricio Jones, DO1. P1925 - The Black Esophagus: A Case of Acute Esophageal Necrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
