Monday Poster Session
Category: Functional Bowel Disease
P1942 - Do Symptoms and Quality of Life Differ Between Patients with Irritable Bowel Syndrome-Diarrhea With Positive vs Negative Hydrogen Breath Test for Small Intestinal Bacterial Overgrowth?
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- BN
Borko Nojkov, MD
University of Michigan
Ann Arbor, Michigan
Presenting Author(s)
Sam Chey, MSc1, Will Takakura, MD1, William D. Chey, MD1, Jason Baker, PhD2, Borko Nojkov, MD1
1University of Michigan, Ann Arbor, MI; 2Anxrobotics, Foley, AL
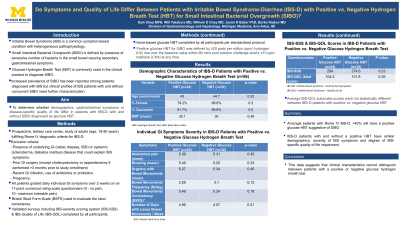
Introduction: IBS is a highly prevalent symptom-based condition with a heterogeneous pathophysiology. Increased prevalence of SIBO has been reported in IBS patients but clinical profiles of IBS patients with and without concurrent SIBO need further characterization. This study aims to determine whether demographics, gastrointestinal symptoms or disease-specific quality of life differ in patients with IBS-D with and without SIBO assessed by glucose HBT.
Methods: Prospective, tertiary-care center, study of adults fulfilling Rome IV criteria for IBS-D. Patients with underlying GI (e.g. IBD) or systemic (e.g. scleroderma) disease that could explain IBS symptoms were excluded. Other exclusion criteria were: pregnancy, prior GI surgery, recent GI infection, use of antibiotics or probiotics. All patients graded their daily individual IBS symptoms for at least 2 weeks on an 11-point numerical rating scale questionnaire (e.g. 0-no pain, 10-max pain). Stool consistency was assessed with Bristol Stool Form Scale. Validated surveys including IBS-severity scoring system (IBS-SSS) and IBS-Quality of Life (IBS-QOL) were also completed. Home-based glucose HBT was completed by all participants per standardized protocol. Positive glucose HBT for SIBO was defined by ≥20 parts per million/ppm hydrogen (H2) rise over the baseline value within 90 mins post solution challenge and/or ≥10 ppm methane (CH4) at any time.
Results: 56 patients completed this ongoing study (mean age 44 yrs, 73% female, 91% Caucasian, mean BMI 30.1). The positivity rate for glucose HBTs was 43% (24/56). Demographic characteristics of patients with positive vs. negative HBT were similar although patients with positive glucose HBT trended to be slightly younger and female. There were no statistically significant differences in average daily IBS individual symptoms scores, nor in daily stool frequency and consistency scores, between patients with positive vs. negative HBT (Table 1). IBS-SSS scores also did not significantly differ between the groups. Similarly, average IBS-QOL total and subscale scores were similar between patients with positive vs. negative glucose HBT.
Discussion: Amongst patients with Rome IV IBS-D, >40% will have a positive glucose HBT suggestive of SIBO. IBS-D patients with and without a positive HBT have similar demographics, severity of IBS symptoms and degree of IBS-specific quality of life impairment. This data suggests that clinical characteristics cannot distinguish between those with a positive or negative breath test.
Disclosures:
Sam Chey, MSc1, Will Takakura, MD1, William D. Chey, MD1, Jason Baker, PhD2, Borko Nojkov, MD1. P1942 - Do Symptoms and Quality of Life Differ Between Patients with Irritable Bowel Syndrome-Diarrhea With Positive vs Negative Hydrogen Breath Test for Small Intestinal Bacterial Overgrowth?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2Anxrobotics, Foley, AL
Introduction: IBS is a highly prevalent symptom-based condition with a heterogeneous pathophysiology. Increased prevalence of SIBO has been reported in IBS patients but clinical profiles of IBS patients with and without concurrent SIBO need further characterization. This study aims to determine whether demographics, gastrointestinal symptoms or disease-specific quality of life differ in patients with IBS-D with and without SIBO assessed by glucose HBT.
Methods: Prospective, tertiary-care center, study of adults fulfilling Rome IV criteria for IBS-D. Patients with underlying GI (e.g. IBD) or systemic (e.g. scleroderma) disease that could explain IBS symptoms were excluded. Other exclusion criteria were: pregnancy, prior GI surgery, recent GI infection, use of antibiotics or probiotics. All patients graded their daily individual IBS symptoms for at least 2 weeks on an 11-point numerical rating scale questionnaire (e.g. 0-no pain, 10-max pain). Stool consistency was assessed with Bristol Stool Form Scale. Validated surveys including IBS-severity scoring system (IBS-SSS) and IBS-Quality of Life (IBS-QOL) were also completed. Home-based glucose HBT was completed by all participants per standardized protocol. Positive glucose HBT for SIBO was defined by ≥20 parts per million/ppm hydrogen (H2) rise over the baseline value within 90 mins post solution challenge and/or ≥10 ppm methane (CH4) at any time.
Results: 56 patients completed this ongoing study (mean age 44 yrs, 73% female, 91% Caucasian, mean BMI 30.1). The positivity rate for glucose HBTs was 43% (24/56). Demographic characteristics of patients with positive vs. negative HBT were similar although patients with positive glucose HBT trended to be slightly younger and female. There were no statistically significant differences in average daily IBS individual symptoms scores, nor in daily stool frequency and consistency scores, between patients with positive vs. negative HBT (Table 1). IBS-SSS scores also did not significantly differ between the groups. Similarly, average IBS-QOL total and subscale scores were similar between patients with positive vs. negative glucose HBT.
Discussion: Amongst patients with Rome IV IBS-D, >40% will have a positive glucose HBT suggestive of SIBO. IBS-D patients with and without a positive HBT have similar demographics, severity of IBS symptoms and degree of IBS-specific quality of life impairment. This data suggests that clinical characteristics cannot distinguish between those with a positive or negative breath test.
Disclosures:
Sam Chey indicated no relevant financial relationships.
Will Takakura indicated no relevant financial relationships.
William D. Chey: Commonwealth Diagnostics International – Grant/Research Support. Salix Pharmaceuticals – Advisor or Review Panel Member, Grant/Research Support.
Jason Baker indicated no relevant financial relationships.
Borko Nojkov indicated no relevant financial relationships.
Sam Chey, MSc1, Will Takakura, MD1, William D. Chey, MD1, Jason Baker, PhD2, Borko Nojkov, MD1. P1942 - Do Symptoms and Quality of Life Differ Between Patients with Irritable Bowel Syndrome-Diarrhea With Positive vs Negative Hydrogen Breath Test for Small Intestinal Bacterial Overgrowth?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
