Monday Poster Session
Category: Functional Bowel Disease
P1962 - Telehealth Is Effective in Delivering Pelvic Floor Physical Therapy in Patients with Pelvic Floor Disorders
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Elisa Karhu, MD, MS
Stanford University
Stanford, CA
Presenting Author(s)
Elisa Karhu, MD, MS1, Julia Barten, DPT2, Gloria Yi, DPT2, Yasir R. Rajwana, MD3, Brooke Gurland, MD4, Leila Neshatian, MD, MSc5
1Stanford University, Stanford, CA; 2Stanford Health Care, Redwood City, CA; 3Stanford Healthcare, Palo Alto, CA; 4Stanford University, Redwood City, CA; 5Stanford, Redwood City, CA
Introduction: Pelvic floor physical therapy (PFPT) is recommended for management of pelvic floor disorders (PFD) including functional defecatory disorders and fecal incontinence. Telehealth utilization, largely spurred by COVID-19 pandemic, has become preferred due to convenience and access. We aimed to assess the effectiveness of telehealth for delivering PFPT.
Methods: In this IRB approved, cross-sectional study, 812 patients who had undergone PFPT by telemedicine or in combination with in-person visits were surveyed. Patient Global Impression of Change (PGIC) was used to analyze post intervention effectiveness.
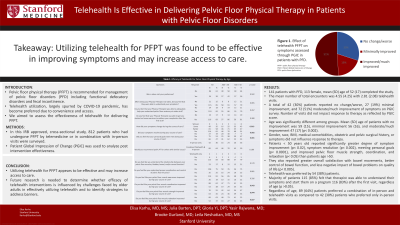
Results: 141 patients with PFD, 113 female, mean (SD) age of 52 (17) completed the study. The mean number of total encounters was 4.55 (4.25) with 2.81 (2.08) telehealth visits. A total of 42 (30%) patients reported no change/worse, 27 (19%) minimal improvement, and 72 (51%) moderate/much improvement of symptoms on PGIC survey. Number of visits did not impact response to therapy as reflected by PGIC score. Age was significantly different among groups. Mean (SD) age of patients with no improvement was 59 (15), minimal improvement 56 (16), and moderate/much improvement 47 (17) (p< 0.002). Gender, race, BMI, medical comorbidities, obstetric and pelvic surgical history, or symptoms did not influence response to therapy. Patients < 50 years old reported significantly greater degree of symptom improvement (p< 0.02), symptom resolution (p< 0.002), meeting personal goals (p< 0.0001), and improved pelvic floor muscle strength, coordination, and relaxation (p< 0.05) than patients age >50. They also reported greater overall satisfaction with bowel movements, better control of bowel function, and less negative impact of bowel problems on quality of life (p< 0.005). Telehealth was preferred by 54 (38%) patients. Majority of patients 115 (85%) felt that therapist was able to understand their symptoms and start them on a program 116 (83%) after the first visit, regardless of age (p >0.05). Regardless of age, 89 (64%) patients preferred a combination of in-person and telehealth visits as compared to 42 (30%) patients who preferred only in-person visits.
Discussion: Utilizing telehealth for PFPT appears to be effective and may increase access to care. Future research is needed to determine whether efficacy of telehealth interventions is influenced by challenges faced by older adults in effectively utilizing telehealth and to identify strategies to address barriers.
Disclosures:
Elisa Karhu, MD, MS1, Julia Barten, DPT2, Gloria Yi, DPT2, Yasir R. Rajwana, MD3, Brooke Gurland, MD4, Leila Neshatian, MD, MSc5. P1962 - Telehealth Is Effective in Delivering Pelvic Floor Physical Therapy in Patients with Pelvic Floor Disorders, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Stanford University, Stanford, CA; 2Stanford Health Care, Redwood City, CA; 3Stanford Healthcare, Palo Alto, CA; 4Stanford University, Redwood City, CA; 5Stanford, Redwood City, CA
Introduction: Pelvic floor physical therapy (PFPT) is recommended for management of pelvic floor disorders (PFD) including functional defecatory disorders and fecal incontinence. Telehealth utilization, largely spurred by COVID-19 pandemic, has become preferred due to convenience and access. We aimed to assess the effectiveness of telehealth for delivering PFPT.
Methods: In this IRB approved, cross-sectional study, 812 patients who had undergone PFPT by telemedicine or in combination with in-person visits were surveyed. Patient Global Impression of Change (PGIC) was used to analyze post intervention effectiveness.
Results: 141 patients with PFD, 113 female, mean (SD) age of 52 (17) completed the study. The mean number of total encounters was 4.55 (4.25) with 2.81 (2.08) telehealth visits. A total of 42 (30%) patients reported no change/worse, 27 (19%) minimal improvement, and 72 (51%) moderate/much improvement of symptoms on PGIC survey. Number of visits did not impact response to therapy as reflected by PGIC score. Age was significantly different among groups. Mean (SD) age of patients with no improvement was 59 (15), minimal improvement 56 (16), and moderate/much improvement 47 (17) (p< 0.002). Gender, race, BMI, medical comorbidities, obstetric and pelvic surgical history, or symptoms did not influence response to therapy. Patients < 50 years old reported significantly greater degree of symptom improvement (p< 0.02), symptom resolution (p< 0.002), meeting personal goals (p< 0.0001), and improved pelvic floor muscle strength, coordination, and relaxation (p< 0.05) than patients age >50. They also reported greater overall satisfaction with bowel movements, better control of bowel function, and less negative impact of bowel problems on quality of life (p< 0.005). Telehealth was preferred by 54 (38%) patients. Majority of patients 115 (85%) felt that therapist was able to understand their symptoms and start them on a program 116 (83%) after the first visit, regardless of age (p >0.05). Regardless of age, 89 (64%) patients preferred a combination of in-person and telehealth visits as compared to 42 (30%) patients who preferred only in-person visits.
Discussion: Utilizing telehealth for PFPT appears to be effective and may increase access to care. Future research is needed to determine whether efficacy of telehealth interventions is influenced by challenges faced by older adults in effectively utilizing telehealth and to identify strategies to address barriers.
Disclosures:
Elisa Karhu indicated no relevant financial relationships.
Julia Barten indicated no relevant financial relationships.
Gloria Yi indicated no relevant financial relationships.
Yasir Rajwana indicated no relevant financial relationships.
Brooke Gurland: Axionics, Intuitive, Cook – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau.
Leila Neshatian: salix, Ardelyx, GI supply, Vibrant – Advisory Committee/Board Member, Consultant.
Elisa Karhu, MD, MS1, Julia Barten, DPT2, Gloria Yi, DPT2, Yasir R. Rajwana, MD3, Brooke Gurland, MD4, Leila Neshatian, MD, MSc5. P1962 - Telehealth Is Effective in Delivering Pelvic Floor Physical Therapy in Patients with Pelvic Floor Disorders, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

