Monday Poster Session
Category: General Endoscopy
P1982 - Redefining Giant: A Systematic Review of Large Gastric Lipomas Since 2017
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Otoniel Hill, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Otoniel Ysea Hill, MD, Bahar Adeli, MD, Afshin Parsikia, MD, Radi Zaki, MD
Albert Einstein Medical Center, Philadelphia, PA
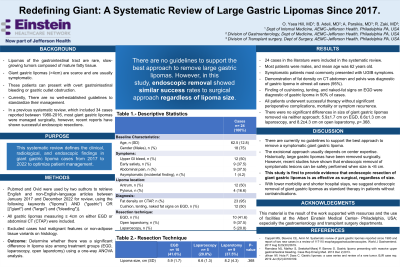
Introduction: Gastric lipomas are asymptomatic, benign tumors comprising < 1-3% of all gastric tumors. Diagnostic criteria or management guidelines based on tumor size are lacking in the literature. Most commonly presenting as an upper gastrointestinal bleed (UGIB) or gastric outlet obstruction (GOO), giant gastric lipomas (GGL) ≥ 4 cm represent a rare subset, with 34 cases reported between 1980-2016. In a previous systematic review, most GGLs were managed surgically; however, recent reports have shown successful endoscopic resections. This systematic review defines the clinical, radiological, and endoscopic findings in GGL cases since 2017 to optimize patient management.
Methods: Pubmed and Ovid were used by two authors to retrieve English and non-English-language articles between January 2017 and December 2022 for review, using the following keywords ("lipoma") AND ("gastric") OR [("giant") and ("large") and ("bleeding")]. All gastric lipomas measuring ≥ 4cm on either EGD or abdominal CT (CTAP) were included. Excluded cases had malignant features or non-adipose tissue variants on histology.
Results: Included cases (n=24) were 75% male, aged 62.5±12.8 years. The mean lipoma size was 7.0±3.0 cm. Most were found in the antral submucosa (n=12). UGIB (n=12), early satiety (n=9), and abdominal pain (n=9) were the most common symptoms at presentation. Mean hemoglobin was 8.3±2.2 g/dL, and four patients required blood transfusions. An EGD was performed before imaging in 75% of patients. Fat density was diagnostic on 95% of all CTAPs performed. On EGD, cushioning, tenting, and naked-fat signs were diagnostic of GGLs in 50% of cases. Two patients had evidence of GOO on EGD. 52% of patients had an endoscopic ultrasound showing a characteristic hyperechoic mass in the third layer. FNA and forceps biopsy were nondiagnostic in 58% of cases. All patients underwent successful therapy without mortality or symptom recurrence. Therapies included removal via EGD (n=10), open laparotomies (n=9), and laparoscopy (n=5). Endoscopic submucosal dissection was the most common EGD approach (n=6). There were no significant differences in the size of GGL removed via either approach; 5.9±1.7 cm on EGD, 6.6±1.3 cm on laparoscopy, and 8.2±4.3 cm on open laparotomy, p=.368.
Discussion: This systematic review is the first to provide evidence that EGD resection of GGL is as effective as surgical removal. With lower morbidity and shorter hospital stays, we suggest this as standard therapy in patients without contraindications.
Disclosures:
Otoniel Ysea Hill, MD, Bahar Adeli, MD, Afshin Parsikia, MD, Radi Zaki, MD. P1982 - Redefining Giant: A Systematic Review of Large Gastric Lipomas Since 2017, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Albert Einstein Medical Center, Philadelphia, PA
Introduction: Gastric lipomas are asymptomatic, benign tumors comprising < 1-3% of all gastric tumors. Diagnostic criteria or management guidelines based on tumor size are lacking in the literature. Most commonly presenting as an upper gastrointestinal bleed (UGIB) or gastric outlet obstruction (GOO), giant gastric lipomas (GGL) ≥ 4 cm represent a rare subset, with 34 cases reported between 1980-2016. In a previous systematic review, most GGLs were managed surgically; however, recent reports have shown successful endoscopic resections. This systematic review defines the clinical, radiological, and endoscopic findings in GGL cases since 2017 to optimize patient management.
Methods: Pubmed and Ovid were used by two authors to retrieve English and non-English-language articles between January 2017 and December 2022 for review, using the following keywords ("lipoma") AND ("gastric") OR [("giant") and ("large") and ("bleeding")]. All gastric lipomas measuring ≥ 4cm on either EGD or abdominal CT (CTAP) were included. Excluded cases had malignant features or non-adipose tissue variants on histology.
Results: Included cases (n=24) were 75% male, aged 62.5±12.8 years. The mean lipoma size was 7.0±3.0 cm. Most were found in the antral submucosa (n=12). UGIB (n=12), early satiety (n=9), and abdominal pain (n=9) were the most common symptoms at presentation. Mean hemoglobin was 8.3±2.2 g/dL, and four patients required blood transfusions. An EGD was performed before imaging in 75% of patients. Fat density was diagnostic on 95% of all CTAPs performed. On EGD, cushioning, tenting, and naked-fat signs were diagnostic of GGLs in 50% of cases. Two patients had evidence of GOO on EGD. 52% of patients had an endoscopic ultrasound showing a characteristic hyperechoic mass in the third layer. FNA and forceps biopsy were nondiagnostic in 58% of cases. All patients underwent successful therapy without mortality or symptom recurrence. Therapies included removal via EGD (n=10), open laparotomies (n=9), and laparoscopy (n=5). Endoscopic submucosal dissection was the most common EGD approach (n=6). There were no significant differences in the size of GGL removed via either approach; 5.9±1.7 cm on EGD, 6.6±1.3 cm on laparoscopy, and 8.2±4.3 cm on open laparotomy, p=.368.
Discussion: This systematic review is the first to provide evidence that EGD resection of GGL is as effective as surgical removal. With lower morbidity and shorter hospital stays, we suggest this as standard therapy in patients without contraindications.
Disclosures:
Otoniel Ysea Hill indicated no relevant financial relationships.
Bahar Adeli indicated no relevant financial relationships.
Afshin Parsikia indicated no relevant financial relationships.
Radi Zaki indicated no relevant financial relationships.
Otoniel Ysea Hill, MD, Bahar Adeli, MD, Afshin Parsikia, MD, Radi Zaki, MD. P1982 - Redefining Giant: A Systematic Review of Large Gastric Lipomas Since 2017, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
