Monday Poster Session
Category: General Endoscopy
P1997 - Ulceration of the Nissen Fundoplication Wrap: An Uncommon Late Complication
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kwabena O. Asafo-Agyei, MD
Christus Highland Hospital
Shreveport, LA
Presenting Author(s)
Kwabena O. Asafo-Agyei, MD1, John Kirkikis, MD2, Dustin Hadley, PA-C3, Prince Djan, MD4
1Christus Highland Hospital, Shreveport, LA; 2GastroIntestinal Specialists, Shreveport, LA; 3GastroIntestinal Specialist, Shreveport, LA; 4SOVAH Health, Martinsville, VA
Introduction: Laparoscopic Nissen fundoplication is a widely used, safe, and effective therapy for gastroesophageal reflux disease (GERD). Gastric ulceration post-procedure is a rare late outcome. Vascular mechanic changes caused by the procedure, non-steroidal anti-inflammatory drugs (NSAIDs), and Helicobacter pylori are well-established causes of ulceration in this group.
Case Description/Methods: A 23-year-old male with a surgical history including Laparoscopic Nissen Fundoplication and cholecystectomy a year ago was admitted with a 3-day episode of black and tarry stools. The patient endorsed taking NSAIDs daily for over a week for worsening epigastric pain. He denied any hematemesis, hematochezia, and no other source of bleeding. On examination, the patient had normal hemodynamics and abdominal examination. Work-up revealed hemoglobin of 11.9 g/dl and hematocrit of 33.2% with normal platelet count.
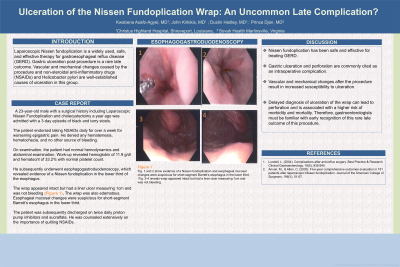
He subsequently underwent esophagogastroduodenoscopy, which revealed evidence of a Nissen fundoplication in the lower third of the esophagus. The wrap appeared intact but had a liner ulcer measuring 1cm and was not bleeding (Figure 1). The wrap was also edematous. Esophageal mucosal changes were suspicious for short-segment Barrett’s esophagus in the lower third.
The patient was subsequently discharged on twice daily proton pump inhibitors and sucralfate. He was counseled extensively on the importance of quitting NSAIDs.
Discussion: Nissen fundoplication has been safe and effective for treating GERD. Gastric ulceration and perforation are commonly cited as an intraoperative complication. Vascular mechanical changes after the procedure result in increased susceptibility to ulceration.
Delayed diagnosis of ulceration of the wrap can lead to perforation and is associated with a higher risk of morbidity and mortality. Therefore, gastroenterologists must be familiar with early recognition of this rare late outcome of this procedure.

Disclosures:
Kwabena O. Asafo-Agyei, MD1, John Kirkikis, MD2, Dustin Hadley, PA-C3, Prince Djan, MD4. P1997 - Ulceration of the Nissen Fundoplication Wrap: An Uncommon Late Complication, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Christus Highland Hospital, Shreveport, LA; 2GastroIntestinal Specialists, Shreveport, LA; 3GastroIntestinal Specialist, Shreveport, LA; 4SOVAH Health, Martinsville, VA
Introduction: Laparoscopic Nissen fundoplication is a widely used, safe, and effective therapy for gastroesophageal reflux disease (GERD). Gastric ulceration post-procedure is a rare late outcome. Vascular mechanic changes caused by the procedure, non-steroidal anti-inflammatory drugs (NSAIDs), and Helicobacter pylori are well-established causes of ulceration in this group.
Case Description/Methods: A 23-year-old male with a surgical history including Laparoscopic Nissen Fundoplication and cholecystectomy a year ago was admitted with a 3-day episode of black and tarry stools. The patient endorsed taking NSAIDs daily for over a week for worsening epigastric pain. He denied any hematemesis, hematochezia, and no other source of bleeding. On examination, the patient had normal hemodynamics and abdominal examination. Work-up revealed hemoglobin of 11.9 g/dl and hematocrit of 33.2% with normal platelet count.
He subsequently underwent esophagogastroduodenoscopy, which revealed evidence of a Nissen fundoplication in the lower third of the esophagus. The wrap appeared intact but had a liner ulcer measuring 1cm and was not bleeding (Figure 1). The wrap was also edematous. Esophageal mucosal changes were suspicious for short-segment Barrett’s esophagus in the lower third.
The patient was subsequently discharged on twice daily proton pump inhibitors and sucralfate. He was counseled extensively on the importance of quitting NSAIDs.
Discussion: Nissen fundoplication has been safe and effective for treating GERD. Gastric ulceration and perforation are commonly cited as an intraoperative complication. Vascular mechanical changes after the procedure result in increased susceptibility to ulceration.
Delayed diagnosis of ulceration of the wrap can lead to perforation and is associated with a higher risk of morbidity and mortality. Therefore, gastroenterologists must be familiar with early recognition of this rare late outcome of this procedure.

Figure: fig 1 and 2 shows evidence of a Nissen fundoplication and esophageal mucosal changes were suspicious for short-segment Barrett’s esophagus in the lower third.
fig3-5 reveals wrap appeared intact but had a liner ulcer measuring 1cm and was not bleeding
fig3-5 reveals wrap appeared intact but had a liner ulcer measuring 1cm and was not bleeding
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
John Kirkikis indicated no relevant financial relationships.
Dustin Hadley indicated no relevant financial relationships.
Prince Djan indicated no relevant financial relationships.
Kwabena O. Asafo-Agyei, MD1, John Kirkikis, MD2, Dustin Hadley, PA-C3, Prince Djan, MD4. P1997 - Ulceration of the Nissen Fundoplication Wrap: An Uncommon Late Complication, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
