Monday Poster Session
Category: General Endoscopy
P2002 - Gastric Amyloidosis as the Cause of Chronic Recurrent Regurgitation – A Description of Novel Endoscopic Findings
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KD
Kathryn Driggers, MD
Walter Reed National Military Medical Center
Bethesda, Maryland
Presenting Author(s)
Kathryn Driggers, MD, Robert Spiller, DO, Danielle D'Ambrosio, MD, Katharine Salyer, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Vomiting and inability to tolerate oral intake are common presenting complaints with broad differential diagnoses. Establishing the source of these symptoms can be challenging, and not all etiologies originate in the gastrointestinal (GI) tract. Gastroparesis is one cause and is relatively common. We present a case of progressive regurgitation and subsequent failure to thrive in a 91-year-old woman.
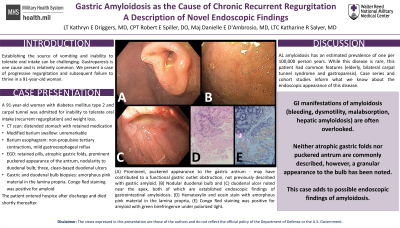
Case Description/Methods: A 91-year-old woman with diabetes mellitus type 2 and carpal tunnel syndrome presented for inability to tolerate oral intake. She was admitted three times for evaluation of regurgitation and continued weight loss. CT scan demonstrated a distended stomach with retained medication, a modified barium swallow was unremarkable, and a barium esophagram revealed a normal esophagus but non-propulsive tertiary contractions and mild gastroesophageal reflux. EGD showed retained pills, atrophic gastric folds, prominent puckered appearance of the antrum, nodularity to the duodenal bulb and three, clean-based duodenal ulcers. The patient was discharged on a proton pump inhibitor twice daily. Biopsies taken from the gastric antrum, incisura, greater curvature and duodenal mucosa adjacent to the ulcers all noted an amorphous pink material in the lamina propria. Congo Red staining was positive for amyloid (likely AL amyloid given her negative M-spike and positive kappa light chains). No further diagnostic testing was pursued due to the patient’s advancing debility and prognosis. The patient passed away shortly after discharge.
Discussion: The epidemiology of AL amyloidosis is challenging to quantify given protean manifestations of the disease but has an estimated prevalence of one per 100,000 person years. Reviews recommend consideration of amyloidosis in patients with kidney dysfunction, cardiomegaly, and/or neuropathy; however, GI manifestations are often overlooked. These include bleeding, dysmotility, malabsorption, and hepatic amyloidosis. This patient had common features (elderly, bilateral carpal tunnel syndrome and gastroparesis) of an uncommon disease. Information about the endoscopic appearance of GI amyloidosis is scarce, with case series and cohort studies forming the body of this evidence. Neither atrophic gastric folds nor puckered antrum are commonly described, however, a granular appearance to the bulb has been noted. We present this case to add to possible endoscopic findings of this disease and highlight the need for further research in this area.

Disclosures:
Kathryn Driggers, MD, Robert Spiller, DO, Danielle D'Ambrosio, MD, Katharine Salyer, MD. P2002 - Gastric Amyloidosis as the Cause of Chronic Recurrent Regurgitation – A Description of Novel Endoscopic Findings, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Vomiting and inability to tolerate oral intake are common presenting complaints with broad differential diagnoses. Establishing the source of these symptoms can be challenging, and not all etiologies originate in the gastrointestinal (GI) tract. Gastroparesis is one cause and is relatively common. We present a case of progressive regurgitation and subsequent failure to thrive in a 91-year-old woman.
Case Description/Methods: A 91-year-old woman with diabetes mellitus type 2 and carpal tunnel syndrome presented for inability to tolerate oral intake. She was admitted three times for evaluation of regurgitation and continued weight loss. CT scan demonstrated a distended stomach with retained medication, a modified barium swallow was unremarkable, and a barium esophagram revealed a normal esophagus but non-propulsive tertiary contractions and mild gastroesophageal reflux. EGD showed retained pills, atrophic gastric folds, prominent puckered appearance of the antrum, nodularity to the duodenal bulb and three, clean-based duodenal ulcers. The patient was discharged on a proton pump inhibitor twice daily. Biopsies taken from the gastric antrum, incisura, greater curvature and duodenal mucosa adjacent to the ulcers all noted an amorphous pink material in the lamina propria. Congo Red staining was positive for amyloid (likely AL amyloid given her negative M-spike and positive kappa light chains). No further diagnostic testing was pursued due to the patient’s advancing debility and prognosis. The patient passed away shortly after discharge.
Discussion: The epidemiology of AL amyloidosis is challenging to quantify given protean manifestations of the disease but has an estimated prevalence of one per 100,000 person years. Reviews recommend consideration of amyloidosis in patients with kidney dysfunction, cardiomegaly, and/or neuropathy; however, GI manifestations are often overlooked. These include bleeding, dysmotility, malabsorption, and hepatic amyloidosis. This patient had common features (elderly, bilateral carpal tunnel syndrome and gastroparesis) of an uncommon disease. Information about the endoscopic appearance of GI amyloidosis is scarce, with case series and cohort studies forming the body of this evidence. Neither atrophic gastric folds nor puckered antrum are commonly described, however, a granular appearance to the bulb has been noted. We present this case to add to possible endoscopic findings of this disease and highlight the need for further research in this area.

Figure: (A) Prominent, puckered appearance to the gastric antrum which may have contributed to a functional gastric outlet obstruction and has not been previously described with gastric amyloid. (B) Nodular duodenal bulb and (C) duodenal ulcer noted near the apex, both of which are established endoscopic findings of gastrointestinal amyloidosis. (D) Hematoxylin and eosin stain with amorphous pink material in the lamina propria, (E) Congo Red staining was positive for amyloid with green birefringence under polarized light.
Disclosures:
Kathryn Driggers indicated no relevant financial relationships.
Robert Spiller indicated no relevant financial relationships.
Danielle D'Ambrosio indicated no relevant financial relationships.
Katharine Salyer indicated no relevant financial relationships.
Kathryn Driggers, MD, Robert Spiller, DO, Danielle D'Ambrosio, MD, Katharine Salyer, MD. P2002 - Gastric Amyloidosis as the Cause of Chronic Recurrent Regurgitation – A Description of Novel Endoscopic Findings, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
