Monday Poster Session
Category: General Endoscopy
P2007 - A Case of Parvimonas micra Bacteremia in a Patient After Esophagogastroduodenoscopy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HR
Hasan S. Raza, MD
University of Illinois Chicago
Chicago, IL
Presenting Author(s)
Hasan Raza, MD1, James Love, MD2, Adam E. Mikolajczyk, MD3
1University of Illinois Chicago, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3University of Illinois Chicago, Highland, IN
Introduction: Parvimonas micra (P. micra) is an anaerobic gram-positive cocci part of the normal flora of the gastrointestinal (GI). P. micra bacteremia has been rarely reported in patients with GI malignancies, such as esophageal and colorectal carcinoma, and underlying periodontal disease. Studies have also shown that acute or chronic liver failure predisposes patients to bacteremia. We present a novel case of P. micra bacteremia in a patient with liver disease admitted for GI bleeding without underlying periodontal disease or malignancy.
Case Description/Methods: A 38-year-old man presented with abdominal pain and emesis for 4 days after taking an unknown quantity of acetaminophen after a physical altercation in conjunction with daily alcohol use. Physical exam was notable for scleral icterus, diffuse abdominal tenderness, and normal dentition. Laboratory findings were consistent with acute liver injury (aspartate transaminase 77 U/L, alanine transaminase 742 U/L, total bilirubin 21.6 mg/dL, PT 20.5 s). Ultrasound revealed increased echogenicity of liver parenchyma and CT revealed small volume ascites. On day 4 of hospitalization, he had an episode of melenic stool and became hemodynamically unstable. Esophagogastroduodenoscopy (EGD) revealed Los Angeles grade D esophagitis and a Mallory-Weiss tear at the gastroesophageal (GE) junction with active bleeding, treated with a hemostatic clip. Two blood cultures drawn 5 days after the GI bleed came back positive for P. micra with subsequent ones negative. Our patient was treated with ampicillin-sulbactam followed by penicillin G for a 14-day course. Transthoracic echocardiogram was normal. Patient followed up in clinic and is doing well.
Discussion: P. Micra most commonly causes infections in immunocompromised hosts. Interestingly, studies suggest an association between tumor colonization of P. micra and tumor immunity in colorectal carcinoma. Our patient was not due for a screening colonoscopy nor did his history of present illness suggest underlying malignancy. The most likely source of bacteremia in this case appears to be due to GI bleeding and associated EGD instrumentation causing translocation of P. micra from the GI tract into the bloodstream in the setting of acute on chronic liver disease. Regardless of route of transmission, P. micra bacteremia requires treatment to prevent sequelae that are commonly seen with bacteremia such as sepsis, endocarditis, and osteomyelitis. Penicillin and metronidazole remain the drugs of choice in treatment of P. micra.

Disclosures:
Hasan Raza, MD1, James Love, MD2, Adam E. Mikolajczyk, MD3. P2007 - A Case of Parvimonas micra Bacteremia in a Patient After Esophagogastroduodenoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Illinois Chicago, Chicago, IL; 2University of Illinois at Chicago, Chicago, IL; 3University of Illinois Chicago, Highland, IN
Introduction: Parvimonas micra (P. micra) is an anaerobic gram-positive cocci part of the normal flora of the gastrointestinal (GI). P. micra bacteremia has been rarely reported in patients with GI malignancies, such as esophageal and colorectal carcinoma, and underlying periodontal disease. Studies have also shown that acute or chronic liver failure predisposes patients to bacteremia. We present a novel case of P. micra bacteremia in a patient with liver disease admitted for GI bleeding without underlying periodontal disease or malignancy.
Case Description/Methods: A 38-year-old man presented with abdominal pain and emesis for 4 days after taking an unknown quantity of acetaminophen after a physical altercation in conjunction with daily alcohol use. Physical exam was notable for scleral icterus, diffuse abdominal tenderness, and normal dentition. Laboratory findings were consistent with acute liver injury (aspartate transaminase 77 U/L, alanine transaminase 742 U/L, total bilirubin 21.6 mg/dL, PT 20.5 s). Ultrasound revealed increased echogenicity of liver parenchyma and CT revealed small volume ascites. On day 4 of hospitalization, he had an episode of melenic stool and became hemodynamically unstable. Esophagogastroduodenoscopy (EGD) revealed Los Angeles grade D esophagitis and a Mallory-Weiss tear at the gastroesophageal (GE) junction with active bleeding, treated with a hemostatic clip. Two blood cultures drawn 5 days after the GI bleed came back positive for P. micra with subsequent ones negative. Our patient was treated with ampicillin-sulbactam followed by penicillin G for a 14-day course. Transthoracic echocardiogram was normal. Patient followed up in clinic and is doing well.
Discussion: P. Micra most commonly causes infections in immunocompromised hosts. Interestingly, studies suggest an association between tumor colonization of P. micra and tumor immunity in colorectal carcinoma. Our patient was not due for a screening colonoscopy nor did his history of present illness suggest underlying malignancy. The most likely source of bacteremia in this case appears to be due to GI bleeding and associated EGD instrumentation causing translocation of P. micra from the GI tract into the bloodstream in the setting of acute on chronic liver disease. Regardless of route of transmission, P. micra bacteremia requires treatment to prevent sequelae that are commonly seen with bacteremia such as sepsis, endocarditis, and osteomyelitis. Penicillin and metronidazole remain the drugs of choice in treatment of P. micra.

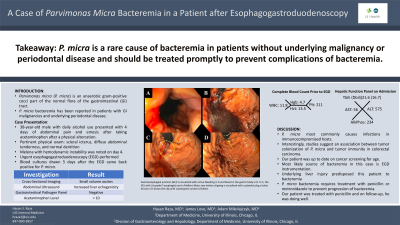
Figure: GE junction is visualized with active bleeding in A and blood in the gastric body in B. In C, the GE junction before clipping is visualized with a platelet plug circled. Arrow in D shows the clip with subsequent control of bleed.
Disclosures:
Hasan Raza indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Adam Mikolajczyk indicated no relevant financial relationships.
Hasan Raza, MD1, James Love, MD2, Adam E. Mikolajczyk, MD3. P2007 - A Case of Parvimonas micra Bacteremia in a Patient After Esophagogastroduodenoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
