Monday Poster Session
Category: GI Bleeding
P2032 - Intermittent vs Continuous PPI Therapy and EGD Timing: A Retrospective Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- VD
Victoria Diaz, MD
Sunrise Health GME Consortium
Las Vegas, NV
Presenting Author(s)
Victoria Diaz, MD1, Youssef Ghobrial, MD1, Pinak Shah, MD1, Kartika Shetty, MD1, Birjees Ahmed, MD1, Napatkamon Ayutyanont, PhD2, Mickayla Clark, PharmD1
1Sunrise Health GME Consortium, Las Vegas, NV; 2GME - Far West Division HCA, Las Vegas, NV
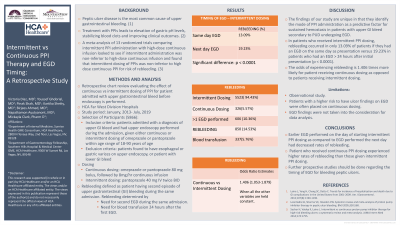
Introduction: Peptic ulcer disease (PUD) is the most common cause of upper gastrointestinal (GI) bleed.
Proton pump inhibitors (PPI) and upper endoscopy are the cornerstone of treatment in patients admitted for peptic ulcer GI bleed.
Current guidelines from the international consensus group recommend esophagogastroduodenoscopy (EGD) within 24 hours of nonvariceal upper GI bleed. This study explores the rates of rebleeding between early and late EGD in patients receiving intermittent versus continuous PPI therapy.
Methods: A retrospective observational study was conducted on HCA far west division hospitals between January 2013 – July 2019. Patients met inclusion criteria if they were 18-90 years of age, admitted with a diagnosis of upper GI bleed and had upper endoscopy performed during the same admission, as well as were given either intermittent or continuous dosing of PPI. Patients were excluded if esophageal or gastric varices were seen on upper endoscopy, or if having a lower GI bleed. Patients received either intermittent dosing of PPI (defined as pantoprazole 40 mg IV BID) and continuous dosing of PPI (defined as pantoprazole 8 mg/hour of continuous IV drip). Patients were then observed for rebleeding (defined as needing a blood transfusion within 24 hours following initial EGD or if a second EGD was needed during the same admission).
Results: A total of 5866 patients were included in the study. 5523 (94.43%) patients received intermittent PPI dosing and 326 (5.57%) patients received continuous PPI dosing. Rebleeding occurred in 850 (14.53%) of patients, with >1 EGD required in 606 (10.36%) and blood transfusion 24 hours after EGD in 337 (5.76%). In patients who received intermittent PPI dosing, rebleeding occurred in 13.09% of patients if they had an EGD on the same day of presentation versus 19.23% in patients who had an EGD > 24 hours after initial presentation, p < 0.0001. Odds ratio for rebleeding in continuous PPI dosing was 1.406 (1.053 -1.879) as opposed to intermittent PPI when all other variables were held constant.
Discussion: Results demonstrate that performing EGD on the day of admission for peptic ulcer bleeding had less rebleeding when compared to EGDs performed > 24 hours later. Continuous PPI dosing had higher rates of rebleeding than intermittent dosing. The findings of our study are unique in that they identify the mode of PPI administration as a predictive factor for sustained hemostasis in patients with upper GI bleed secondary to PUD undergoing EGD.
Disclosures:
Victoria Diaz, MD1, Youssef Ghobrial, MD1, Pinak Shah, MD1, Kartika Shetty, MD1, Birjees Ahmed, MD1, Napatkamon Ayutyanont, PhD2, Mickayla Clark, PharmD1. P2032 - Intermittent vs Continuous PPI Therapy and EGD Timing: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Sunrise Health GME Consortium, Las Vegas, NV; 2GME - Far West Division HCA, Las Vegas, NV
Introduction: Peptic ulcer disease (PUD) is the most common cause of upper gastrointestinal (GI) bleed.
Proton pump inhibitors (PPI) and upper endoscopy are the cornerstone of treatment in patients admitted for peptic ulcer GI bleed.
Current guidelines from the international consensus group recommend esophagogastroduodenoscopy (EGD) within 24 hours of nonvariceal upper GI bleed. This study explores the rates of rebleeding between early and late EGD in patients receiving intermittent versus continuous PPI therapy.
Methods: A retrospective observational study was conducted on HCA far west division hospitals between January 2013 – July 2019. Patients met inclusion criteria if they were 18-90 years of age, admitted with a diagnosis of upper GI bleed and had upper endoscopy performed during the same admission, as well as were given either intermittent or continuous dosing of PPI. Patients were excluded if esophageal or gastric varices were seen on upper endoscopy, or if having a lower GI bleed. Patients received either intermittent dosing of PPI (defined as pantoprazole 40 mg IV BID) and continuous dosing of PPI (defined as pantoprazole 8 mg/hour of continuous IV drip). Patients were then observed for rebleeding (defined as needing a blood transfusion within 24 hours following initial EGD or if a second EGD was needed during the same admission).
Results: A total of 5866 patients were included in the study. 5523 (94.43%) patients received intermittent PPI dosing and 326 (5.57%) patients received continuous PPI dosing. Rebleeding occurred in 850 (14.53%) of patients, with >1 EGD required in 606 (10.36%) and blood transfusion 24 hours after EGD in 337 (5.76%). In patients who received intermittent PPI dosing, rebleeding occurred in 13.09% of patients if they had an EGD on the same day of presentation versus 19.23% in patients who had an EGD > 24 hours after initial presentation, p < 0.0001. Odds ratio for rebleeding in continuous PPI dosing was 1.406 (1.053 -1.879) as opposed to intermittent PPI when all other variables were held constant.
Discussion: Results demonstrate that performing EGD on the day of admission for peptic ulcer bleeding had less rebleeding when compared to EGDs performed > 24 hours later. Continuous PPI dosing had higher rates of rebleeding than intermittent dosing. The findings of our study are unique in that they identify the mode of PPI administration as a predictive factor for sustained hemostasis in patients with upper GI bleed secondary to PUD undergoing EGD.
Disclosures:
Victoria Diaz indicated no relevant financial relationships.
Youssef Ghobrial indicated no relevant financial relationships.
Pinak Shah indicated no relevant financial relationships.
Kartika Shetty indicated no relevant financial relationships.
Birjees Ahmed indicated no relevant financial relationships.
Napatkamon Ayutyanont indicated no relevant financial relationships.
Mickayla Clark indicated no relevant financial relationships.
Victoria Diaz, MD1, Youssef Ghobrial, MD1, Pinak Shah, MD1, Kartika Shetty, MD1, Birjees Ahmed, MD1, Napatkamon Ayutyanont, PhD2, Mickayla Clark, PharmD1. P2032 - Intermittent vs Continuous PPI Therapy and EGD Timing: A Retrospective Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
