Monday Poster Session
Category: GI Bleeding
P2033 - Aortic Stenosis Is Associated With Worse Outcomes in Patients Admitted With Lower Gastrointestinal Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Chidiebele E. Omaliko, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Chidiebele Omaliko, MD1, Favour Markson, MD2, Chukwunonso B. Ezeani, MBBS3, Oghenefejiro Ogwor, MD4, Ayobami Olafimihan, MD5, Chidiebube Ugwu, MD6, Festus O. Ibe, MD7
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Lincoln Medical Center, Bronx, NY; 3Baton Rouge General Hospital, Baton Rouge, LA; 4St. Peters University Hospital, New Brunswick, NJ; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6East Tennessee State University, Johnson City, TN; 7Einstein Medical Center, Philadelphia, PA
Introduction: The association between aortic stenosis (AS) and lower Gastrointestinal bleeding (LGIB) has been described in various studies, however very few reports have described the prognostic implications of lower GI bleeding in patients with AS. Our study aims to ascertain the in-hospital outcomes of AS patients who were admitted to the hospital with a principal diagnosis of lower GI bleeding using a national representative sample.
Methods: A retrospective analysis of patients admitted for Lower GI bleeding from 2016 – 2019 using the National Inpatient Sample (NIS) was conducted. ICD 10 codes were used to Identify individuals with Lower GI bleeding which were further divided into 2 groups based on the presence or absence of a history of AS. Following control for confounders, we compared the risk of in hospital mortality and other outcomes including artery embolization, hypovolemic shock, frequency of blood transfusion, Length of stay and total hospitalization charges amongst both groups.
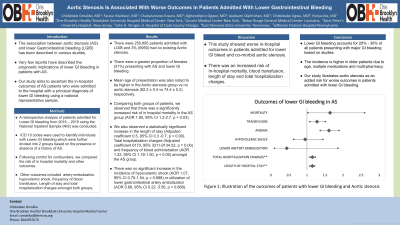
Results: There were 250,895 patients admitted with LGIB and 3% (6950) had co existing Aortic stenosis. There
were a greater proportion of females (51%) presenting with AS and lower GI bleeding. Mean age of
presentation was also noted to be higher in the Aortic stenosis group vs no aortic stenosis (82.2 ± 0.4 vs
74.4 ± 0.2) respectively. Comparing both groups of patients, we observed that there was a significantly increased risk of in hospital
mortality in the AS group (AOR 1.85, 95% CI 1.2-2.7, p = 0.03). We also observed a statistically significant
increase in the length of stay (Adjusted coefficient 0.5, 95% CI 0.3 -0.7, p = 0.00), Total hospitalization
charges (Adjusted coefficient 6173, 95% 3211-9134.52, p = 0.00) and frequency of blood administration
(AOR 1.32, 95% CI 1.16-1.50, p = 0.00) amongst the AS group. There was no significant increase in the
incidence of hypovolemic shock (AOR 1.07, 95% CI 0.75-1.54, p = 0.698) or utilization of lower
gastrointestinal artery embolization (AOR 0.88, 95% CI 0.22 -3.56, p = 0.868).
Discussion: This study showed worse in-hospital outcomes in patients admitted for lower GI bleed and co-morbid
aortic stenosis with an increased risk of In-hospital mortality, blood transfusion, length of stay and total
hospitalization charges.
Disclosures:
Chidiebele Omaliko, MD1, Favour Markson, MD2, Chukwunonso B. Ezeani, MBBS3, Oghenefejiro Ogwor, MD4, Ayobami Olafimihan, MD5, Chidiebube Ugwu, MD6, Festus O. Ibe, MD7. P2033 - Aortic Stenosis Is Associated With Worse Outcomes in Patients Admitted With Lower Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Lincoln Medical Center, Bronx, NY; 3Baton Rouge General Hospital, Baton Rouge, LA; 4St. Peters University Hospital, New Brunswick, NJ; 5John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 6East Tennessee State University, Johnson City, TN; 7Einstein Medical Center, Philadelphia, PA
Introduction: The association between aortic stenosis (AS) and lower Gastrointestinal bleeding (LGIB) has been described in various studies, however very few reports have described the prognostic implications of lower GI bleeding in patients with AS. Our study aims to ascertain the in-hospital outcomes of AS patients who were admitted to the hospital with a principal diagnosis of lower GI bleeding using a national representative sample.
Methods: A retrospective analysis of patients admitted for Lower GI bleeding from 2016 – 2019 using the National Inpatient Sample (NIS) was conducted. ICD 10 codes were used to Identify individuals with Lower GI bleeding which were further divided into 2 groups based on the presence or absence of a history of AS. Following control for confounders, we compared the risk of in hospital mortality and other outcomes including artery embolization, hypovolemic shock, frequency of blood transfusion, Length of stay and total hospitalization charges amongst both groups.
Results: There were 250,895 patients admitted with LGIB and 3% (6950) had co existing Aortic stenosis. There
were a greater proportion of females (51%) presenting with AS and lower GI bleeding. Mean age of
presentation was also noted to be higher in the Aortic stenosis group vs no aortic stenosis (82.2 ± 0.4 vs
74.4 ± 0.2) respectively. Comparing both groups of patients, we observed that there was a significantly increased risk of in hospital
mortality in the AS group (AOR 1.85, 95% CI 1.2-2.7, p = 0.03). We also observed a statistically significant
increase in the length of stay (Adjusted coefficient 0.5, 95% CI 0.3 -0.7, p = 0.00), Total hospitalization
charges (Adjusted coefficient 6173, 95% 3211-9134.52, p = 0.00) and frequency of blood administration
(AOR 1.32, 95% CI 1.16-1.50, p = 0.00) amongst the AS group. There was no significant increase in the
incidence of hypovolemic shock (AOR 1.07, 95% CI 0.75-1.54, p = 0.698) or utilization of lower
gastrointestinal artery embolization (AOR 0.88, 95% CI 0.22 -3.56, p = 0.868).
Discussion: This study showed worse in-hospital outcomes in patients admitted for lower GI bleed and co-morbid
aortic stenosis with an increased risk of In-hospital mortality, blood transfusion, length of stay and total
hospitalization charges.
Disclosures:
Chidiebele Omaliko indicated no relevant financial relationships.
Favour Markson indicated no relevant financial relationships.
Chukwunonso Ezeani indicated no relevant financial relationships.
Oghenefejiro Ogwor indicated no relevant financial relationships.
Ayobami Olafimihan indicated no relevant financial relationships.
Chidiebube Ugwu indicated no relevant financial relationships.
Festus Ibe indicated no relevant financial relationships.
Chidiebele Omaliko, MD1, Favour Markson, MD2, Chukwunonso B. Ezeani, MBBS3, Oghenefejiro Ogwor, MD4, Ayobami Olafimihan, MD5, Chidiebube Ugwu, MD6, Festus O. Ibe, MD7. P2033 - Aortic Stenosis Is Associated With Worse Outcomes in Patients Admitted With Lower Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
