Monday Poster Session
Category: GI Bleeding
P2035 - Gastrointestinal Bleeding Episodes Following Aortic Valve Replacement in Heyde’s Syndrome: A Large Scale Database Study Using TriNetX
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Marguerite O. Linz, MD
Case Western Reserve University, University Hospitals
Cleveland, OH
Presenting Author(s)
Award: Presidential Poster Award
Marguerite O. Linz, MD1, Maurice Facey, MD2, Akash Khurana, MD1, Scott Martin, PhD2, Emad Mansoor, MD3, Jaime A. Perez, PhD4, Gerard Isenberg, MD, MBA1
1Case Western Reserve University, University Hospitals, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Case Western Reserve University / University Hospitals, Cleveland, OH; 4University Hospitals Clinical Research Center, Cleveland, OH
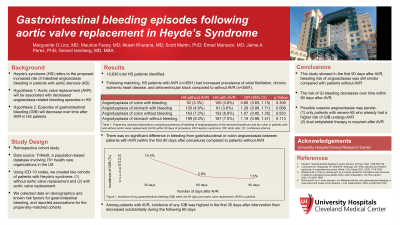
Introduction: Heyde’s syndrome (HS) is defined as the relationship between aortic stenosis (AS) and intestinal angioectasia bleeding. However, it is unclear if aortic valve replacement (AVR) definitively reduces risk of future gastrointestinal bleeding (GIB) in HS. We sought to evaluate whether AVR was associated with decreased angioectasia-related bleeding episodes in HS, and determine whether a relationship exists between duration of time post-AVR and future GIB.
Methods: We conducted a retrospective cohort study using TriNetX, a population-based database that sources data from electronic medical records of 73 health care organizations in the US. Using ICD-10 codes, we created two cohorts of patients with HS: without AVR and with AVR. Within each cohort, we collected data on demographics, and several risk factors for GIB including cardiovascular disorders, renal disease, genetic and acquired bleeding disorders and medications including antiplatelets and anticoagulants, and then performed propensity score matching (PSM) of 25 variables to control for confounding (Table 1). Odds ratio (OR) and 95% confidence interval (CI) were used to report on associations for the propensity-matched cohorts.
Results: HS patients with AVR (n=3357) had increased prevalence of atrial fibrillation, chronic ischemic heart disease, atrioventricular block and ejection fraction >50% (Table 1) compared to without AVR (n=3357). Despite matching, they were older with higher adenosine diphosphate and INR. Compared to patients after AVR, HS patients without AVR were less likely to have bleeding from colon angioectasia (OR 0.750, CI 0.61-0.92, p=0.005). However rates of gastroduodenal angioectasia bleeding were similar among the two cohorts (OR 1.066, CI 0.87-1.31, p=0.546) at any time following index event of AVR. The highest incidence of any GIB after aortic valve replacement was within the first 30 days (14.7%) with a decreased rate of 3.0% at 60 days, then decreased to 1.5% 90 days post-intervention.
Discussion: HS patients with aortic valve replacement unexpectedly have increased bleeding risk of colon angioectasias and similar bleeding risk of gastroduodenal angioectasia compared with HS patients without replacement. Angioectasias may persist after AVR considering that only patients with severe AS who already had a higher risk of GIB undergo AVR. The required dual antiplatelet therapy after AVR may also increase GIB risk. However, the risk of GIB decreases over time within 90 days of AVR.
Disclosures:
Marguerite O. Linz, MD1, Maurice Facey, MD2, Akash Khurana, MD1, Scott Martin, PhD2, Emad Mansoor, MD3, Jaime A. Perez, PhD4, Gerard Isenberg, MD, MBA1. P2035 - Gastrointestinal Bleeding Episodes Following Aortic Valve Replacement in Heyde’s Syndrome: A Large Scale Database Study Using TriNetX, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Marguerite O. Linz, MD1, Maurice Facey, MD2, Akash Khurana, MD1, Scott Martin, PhD2, Emad Mansoor, MD3, Jaime A. Perez, PhD4, Gerard Isenberg, MD, MBA1
1Case Western Reserve University, University Hospitals, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3Case Western Reserve University / University Hospitals, Cleveland, OH; 4University Hospitals Clinical Research Center, Cleveland, OH
Introduction: Heyde’s syndrome (HS) is defined as the relationship between aortic stenosis (AS) and intestinal angioectasia bleeding. However, it is unclear if aortic valve replacement (AVR) definitively reduces risk of future gastrointestinal bleeding (GIB) in HS. We sought to evaluate whether AVR was associated with decreased angioectasia-related bleeding episodes in HS, and determine whether a relationship exists between duration of time post-AVR and future GIB.
Methods: We conducted a retrospective cohort study using TriNetX, a population-based database that sources data from electronic medical records of 73 health care organizations in the US. Using ICD-10 codes, we created two cohorts of patients with HS: without AVR and with AVR. Within each cohort, we collected data on demographics, and several risk factors for GIB including cardiovascular disorders, renal disease, genetic and acquired bleeding disorders and medications including antiplatelets and anticoagulants, and then performed propensity score matching (PSM) of 25 variables to control for confounding (Table 1). Odds ratio (OR) and 95% confidence interval (CI) were used to report on associations for the propensity-matched cohorts.
Results: HS patients with AVR (n=3357) had increased prevalence of atrial fibrillation, chronic ischemic heart disease, atrioventricular block and ejection fraction >50% (Table 1) compared to without AVR (n=3357). Despite matching, they were older with higher adenosine diphosphate and INR. Compared to patients after AVR, HS patients without AVR were less likely to have bleeding from colon angioectasia (OR 0.750, CI 0.61-0.92, p=0.005). However rates of gastroduodenal angioectasia bleeding were similar among the two cohorts (OR 1.066, CI 0.87-1.31, p=0.546) at any time following index event of AVR. The highest incidence of any GIB after aortic valve replacement was within the first 30 days (14.7%) with a decreased rate of 3.0% at 60 days, then decreased to 1.5% 90 days post-intervention.
Discussion: HS patients with aortic valve replacement unexpectedly have increased bleeding risk of colon angioectasias and similar bleeding risk of gastroduodenal angioectasia compared with HS patients without replacement. Angioectasias may persist after AVR considering that only patients with severe AS who already had a higher risk of GIB undergo AVR. The required dual antiplatelet therapy after AVR may also increase GIB risk. However, the risk of GIB decreases over time within 90 days of AVR.
Disclosures:
Marguerite Linz indicated no relevant financial relationships.
Maurice Facey indicated no relevant financial relationships.
Akash Khurana indicated no relevant financial relationships.
Scott Martin indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Gerard Isenberg indicated no relevant financial relationships.
Marguerite O. Linz, MD1, Maurice Facey, MD2, Akash Khurana, MD1, Scott Martin, PhD2, Emad Mansoor, MD3, Jaime A. Perez, PhD4, Gerard Isenberg, MD, MBA1. P2035 - Gastrointestinal Bleeding Episodes Following Aortic Valve Replacement in Heyde’s Syndrome: A Large Scale Database Study Using TriNetX, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.


