Monday Poster Session
Category: GI Bleeding
P2037 - Risk Factors and Outcomes Associated With Colonic Diverticular Bleeding: Results From Nationwide Inpatient Sample Database
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- TW
TJ L. Wilson, MD
Detroit Medical Center/Wayne State University
Detroit, MI
Presenting Author(s)
Tooba Tariq, MD1, TJ L. Wilson, MD1, Anirudh R. Damughatla, DO2, Mohamad I.. Itani, MD1, Majd Khadra, MD1, Bashar Mohamad, MD3
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 3Wayne State University, Detroit, MI
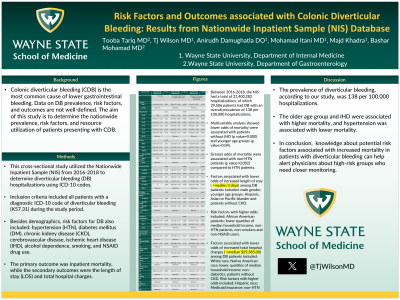
Introduction: Colonic diverticular bleeding (CDB) is the most common cause of lower gastrointestinal bleeding. Data on DB prevalence, risk factors, and outcomes are not well-defined. The aim of this study is to determine the nationwide prevalence, risk factors, and resource utilization of patients presenting with CDB.
Methods: This cross-sectional study utilized the Nationwide Inpatient Sample (NIS) from 2016-2018 to determine diverticular bleeding (DB) hospitalizations using ICD-10 codes. Inclusion criteria included all patients with a diagnostic ICD-10 code of diverticular bleeding (K57.31) during the study period. Besides demographics, risk factors for DB also included: hypertension (HTN), diabetes mellitus (DM), chronic kidney disease (CKD), cerebrovascular disease, ischemic heart disease (IHD), alcohol dependence, smoking, and NSAID drug use. The primary outcome was inpatient mortality, while the secondary outcomes were the length of stay (LOS) and total hospital charges.
Results: Between 2016-2018, the NIS had a total of 21,400,282 hospitalizations, of which 29,506 patients had DB with an overall prevalence of 138 per 100,000 hospitalizations. Multivariable analysis showed lower odds of mortality were associated with patients without IHD (p value=0.000) and younger age groups (p value=0.04). Greater odds of mortality were associated with non-HTN patients (p value=0.002) compared to HTN patients. Factors associated with lower odds of increased length of stay ( >median 3 days) among DB patients included: male gender, younger age groups, Hispanic, Asian or Pacific Islander and patients without CKD. Risk factors with higher odds included: African American patients; lower quartiles of median household income, non-HTN patients, non-smokers and non-NSAID users. Factors associated with lower odds of increased total hospital charges ( >median $29,385.00) among DB patients included: White race, Native American race; lower quartiles of median household income; non-diabetics; patients without CKD. Risk factors with higher odds included: Hispanic race; Medicaid insurance; non-HTN patients.
Discussion: The prevalence of diverticular bleeding, according to our study, was 138 per 100,000 hospitalizations. The older age group and IHD were associated with higher mortality, and hypertension was associated with lower mortality. Knowledge about potential risk factors associated with increased mortality in patients with diverticular bleeding can help alert physicians about high-risk groups who need closer monitoring.
Disclosures:
Tooba Tariq, MD1, TJ L. Wilson, MD1, Anirudh R. Damughatla, DO2, Mohamad I.. Itani, MD1, Majd Khadra, MD1, Bashar Mohamad, MD3. P2037 - Risk Factors and Outcomes Associated With Colonic Diverticular Bleeding: Results From Nationwide Inpatient Sample Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Detroit Medical Center/Wayne State University, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 3Wayne State University, Detroit, MI
Introduction: Colonic diverticular bleeding (CDB) is the most common cause of lower gastrointestinal bleeding. Data on DB prevalence, risk factors, and outcomes are not well-defined. The aim of this study is to determine the nationwide prevalence, risk factors, and resource utilization of patients presenting with CDB.
Methods: This cross-sectional study utilized the Nationwide Inpatient Sample (NIS) from 2016-2018 to determine diverticular bleeding (DB) hospitalizations using ICD-10 codes. Inclusion criteria included all patients with a diagnostic ICD-10 code of diverticular bleeding (K57.31) during the study period. Besides demographics, risk factors for DB also included: hypertension (HTN), diabetes mellitus (DM), chronic kidney disease (CKD), cerebrovascular disease, ischemic heart disease (IHD), alcohol dependence, smoking, and NSAID drug use. The primary outcome was inpatient mortality, while the secondary outcomes were the length of stay (LOS) and total hospital charges.
Results: Between 2016-2018, the NIS had a total of 21,400,282 hospitalizations, of which 29,506 patients had DB with an overall prevalence of 138 per 100,000 hospitalizations. Multivariable analysis showed lower odds of mortality were associated with patients without IHD (p value=0.000) and younger age groups (p value=0.04). Greater odds of mortality were associated with non-HTN patients (p value=0.002) compared to HTN patients. Factors associated with lower odds of increased length of stay ( >median 3 days) among DB patients included: male gender, younger age groups, Hispanic, Asian or Pacific Islander and patients without CKD. Risk factors with higher odds included: African American patients; lower quartiles of median household income, non-HTN patients, non-smokers and non-NSAID users. Factors associated with lower odds of increased total hospital charges ( >median $29,385.00) among DB patients included: White race, Native American race; lower quartiles of median household income; non-diabetics; patients without CKD. Risk factors with higher odds included: Hispanic race; Medicaid insurance; non-HTN patients.
Discussion: The prevalence of diverticular bleeding, according to our study, was 138 per 100,000 hospitalizations. The older age group and IHD were associated with higher mortality, and hypertension was associated with lower mortality. Knowledge about potential risk factors associated with increased mortality in patients with diverticular bleeding can help alert physicians about high-risk groups who need closer monitoring.
Disclosures:
Tooba Tariq indicated no relevant financial relationships.
TJ Wilson indicated no relevant financial relationships.
Anirudh R. Damughatla indicated no relevant financial relationships.
Mohamad Itani indicated no relevant financial relationships.
Majd Khadra indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Tooba Tariq, MD1, TJ L. Wilson, MD1, Anirudh R. Damughatla, DO2, Mohamad I.. Itani, MD1, Majd Khadra, MD1, Bashar Mohamad, MD3. P2037 - Risk Factors and Outcomes Associated With Colonic Diverticular Bleeding: Results From Nationwide Inpatient Sample Database, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
