Monday Poster Session
Category: GI Bleeding
P2043 - The Utility of Charlson Comorbidity Index in Evaluating Patients with Non-Variceal Upper Gastrointestinal Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Khaled Elfert, MD
SBH Health System
Bronx, NY
Presenting Author(s)
Khaled Elfert, MD1, Suut Gokturk, MD2, Vijay Gayam, MD3, Anas Mahmoud, MD4, Azizullah Beran, MD5, Manasik Abdu, MD6, Suresh Nayudu, MD1
1SBH Health System, Bronx, NY; 2SBH, Cheshire, CT; 3Brooklyn Hospital Center, Brooklyn, NY; 4St. Joseph's University Medical Center, Paterson, NJ; 5Indiana University, Indianapolis, IN; 6University at Buffalo-Catholic Health System, Buffalo, NY
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a common medical emergency that has significant morbidity and mortality. Charlson comorbidity index (CCI) is an index that indicates the disease burden based on the weighted score of 17 comorbidities. Our study aims to assess the value of CCI in evaluating the prognosis of patients admitted with NVUGIB.
Methods: We conducted an analysis using the National Inpatient Sample Database from years 2016 to 2019. The study included patients who were admitted to the hospital with a principal diagnosis of NVUGIB. The patients were categorized based on their CCI.
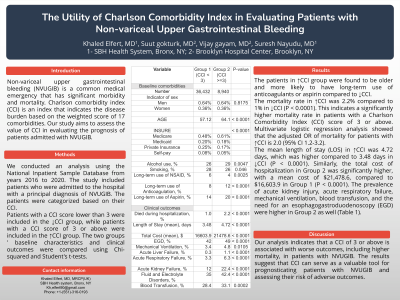
Patients with a CCI score lower than 3 were included in the first group (Group 1), while patients with a CCI score of 3 or above were included in the second group (Group 2). The two groups ' baseline characteristics and clinical outcomes were compared using Chi-squared and Student's t-tests.
Results: 36,432 were included in Group 1, and 8,940 were included in Group 2. No significant differences were found in the gender distribution between the two groups. However, patients in Group 2 were found to be older and more likely to have long-term use of anticoagulants or aspirin compared to Group 1.
The mortality rate in Group 2 was 2.2% compared to 1% in Group 1 (P < 0.0001). This indicates a significantly higher mortality rate in patients with a Charlson Comorbidity Index (CCI) score of 3 or above compared to those with a CCI score lower than 3. Multivariate logistic regression analysis showed that the adjusted OR of mortality for patients with high CCI is 2.0 (95% CI 1.2-3.2).
The mean length of stay (LOS) in Group 2 was 4.72 days, which was higher compared to 3.48 days in Group 1 (P < 0.0001). Similarly, the total cost of hospitalization in Group 2 was significantly higher, with a mean cost of $21,478.6, compared to $16,603.9 in Group 1 (P < 0.0001). The prevalence of acute kidney injury, acute respiratory failure, mechanical ventilation, blood transfusion, and the need for an esophagogastroduodenoscopy (EGD) were higher in Group 2 as well (Table 1).
Discussion: Our analysis indicates that a CCI of 3 or above is associated with worse outcomes, including higher mortality, in patients with NVUGIB. The results suggest that CCI can serve as a valuable tool for prognosticating patients with NVUGIB and assessing their risk of adverse outcomes.
Disclosures:
Khaled Elfert, MD1, Suut Gokturk, MD2, Vijay Gayam, MD3, Anas Mahmoud, MD4, Azizullah Beran, MD5, Manasik Abdu, MD6, Suresh Nayudu, MD1. P2043 - The Utility of Charlson Comorbidity Index in Evaluating Patients with Non-Variceal Upper Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SBH Health System, Bronx, NY; 2SBH, Cheshire, CT; 3Brooklyn Hospital Center, Brooklyn, NY; 4St. Joseph's University Medical Center, Paterson, NJ; 5Indiana University, Indianapolis, IN; 6University at Buffalo-Catholic Health System, Buffalo, NY
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a common medical emergency that has significant morbidity and mortality. Charlson comorbidity index (CCI) is an index that indicates the disease burden based on the weighted score of 17 comorbidities. Our study aims to assess the value of CCI in evaluating the prognosis of patients admitted with NVUGIB.
Methods: We conducted an analysis using the National Inpatient Sample Database from years 2016 to 2019. The study included patients who were admitted to the hospital with a principal diagnosis of NVUGIB. The patients were categorized based on their CCI.
Patients with a CCI score lower than 3 were included in the first group (Group 1), while patients with a CCI score of 3 or above were included in the second group (Group 2). The two groups ' baseline characteristics and clinical outcomes were compared using Chi-squared and Student's t-tests.
Results: 36,432 were included in Group 1, and 8,940 were included in Group 2. No significant differences were found in the gender distribution between the two groups. However, patients in Group 2 were found to be older and more likely to have long-term use of anticoagulants or aspirin compared to Group 1.
The mortality rate in Group 2 was 2.2% compared to 1% in Group 1 (P < 0.0001). This indicates a significantly higher mortality rate in patients with a Charlson Comorbidity Index (CCI) score of 3 or above compared to those with a CCI score lower than 3. Multivariate logistic regression analysis showed that the adjusted OR of mortality for patients with high CCI is 2.0 (95% CI 1.2-3.2).
The mean length of stay (LOS) in Group 2 was 4.72 days, which was higher compared to 3.48 days in Group 1 (P < 0.0001). Similarly, the total cost of hospitalization in Group 2 was significantly higher, with a mean cost of $21,478.6, compared to $16,603.9 in Group 1 (P < 0.0001). The prevalence of acute kidney injury, acute respiratory failure, mechanical ventilation, blood transfusion, and the need for an esophagogastroduodenoscopy (EGD) were higher in Group 2 as well (Table 1).
Discussion: Our analysis indicates that a CCI of 3 or above is associated with worse outcomes, including higher mortality, in patients with NVUGIB. The results suggest that CCI can serve as a valuable tool for prognosticating patients with NVUGIB and assessing their risk of adverse outcomes.
Disclosures:
Khaled Elfert indicated no relevant financial relationships.
Suut Gokturk indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Anas Mahmoud indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Manasik Abdu indicated no relevant financial relationships.
Suresh Nayudu indicated no relevant financial relationships.
Khaled Elfert, MD1, Suut Gokturk, MD2, Vijay Gayam, MD3, Anas Mahmoud, MD4, Azizullah Beran, MD5, Manasik Abdu, MD6, Suresh Nayudu, MD1. P2043 - The Utility of Charlson Comorbidity Index in Evaluating Patients with Non-Variceal Upper Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
