Monday Poster Session
Category: GI Bleeding
P2053 - Unmasking Cameron Lesions: A Rare Etiology of Massive Upper Gastrointestinal Bleeding and Hemodynamic Instability
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Gagan P. Singh, MD
Howard University Hospital
Washington, DC
Presenting Author(s)
Gagan P. Singh, MD1, Justice Arhinful, MD2, Lakshmi Chirumamilla, MD1, Suryanarayana Reddy Challa, MD1, Mukarram Jamat Ali, MD1, Vishal Poddar, MD1
1Howard University Hospital, Washington, DC; 2Howard University, Washington, DC
Introduction: Cameron lesions, while rare and potentially causing severe GI bleeding, are frequently underdiagnosed. They are seen in 5-20% of large hiatal hernia patients, commonly affecting the elderly, with no gender bias. Larger hernias increase the risk. Our case report focuses on a 97-year-old patient's experience with Cameron lesions, from onset marked by hemodynamic instability due to massive upper GI bleeding, through diagnosis and management. This highlights the crucial need for alert identification and prompt intervention.
Case Description/Methods: A 97-year-old female patient arrived at the Emergency Department (ED) with three occurrences of melena and one coffee-ground emesis accompanied by dizziness and light-headedness. A year prior, she was hospitalized for severe symptomatic anemia. An Esophagogastroduodenoscopy (EGD) revealed a large hiatal hernia with non-bleeding superficial gastric ulcers and erosions, identified as the bleeding source. In the ED, she was hypotensive and tachycardic with an initial hemoglobin level of 8.3 g/dL, later dropping to 6.6 g/dL. Melena was confirmed through digital rectal examination. A computed tomography (CT) scan revealed a large sliding hiatal hernia with most of the the stomach's content above the gastroesophageal junction.
Management involved intravenous fluid hydration and two units of packed red blood cells transfusion, raising her hemoglobin to 9.6 g/dL and improving symptoms. Repeat EGD affirmed the presence of Cameron lesions. Despite no active bleeding, a multidisciplinary team evaluated the risks and benefits of surgery, deciding to defer due to her advanced age. She was prescribed pantoprazole, sucralfate, levothyroxine, and hydrochlorothiazide, with a plan to continue proton pump inhibitor therapy indefinitely.
Discussion: Cameron lesions, though rare, can trigger significant morbidity, particularly in older patients with sizable hiatal hernias. Accurate detection necessitates vigilance and a detailed endoscopic examination. Treatment ranges from medical therapy to surgery, based on symptom severity and recurrence. This report underscores the importance of correctly identifying Cameron lesions via symptoms and crafting personalized management plans. These strategies should consider the patient's general health, bleeding intensity, and the potential surgical risks and benefits involved.

Disclosures:
Gagan P. Singh, MD1, Justice Arhinful, MD2, Lakshmi Chirumamilla, MD1, Suryanarayana Reddy Challa, MD1, Mukarram Jamat Ali, MD1, Vishal Poddar, MD1. P2053 - Unmasking Cameron Lesions: A Rare Etiology of Massive Upper Gastrointestinal Bleeding and Hemodynamic Instability, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Howard University Hospital, Washington, DC; 2Howard University, Washington, DC
Introduction: Cameron lesions, while rare and potentially causing severe GI bleeding, are frequently underdiagnosed. They are seen in 5-20% of large hiatal hernia patients, commonly affecting the elderly, with no gender bias. Larger hernias increase the risk. Our case report focuses on a 97-year-old patient's experience with Cameron lesions, from onset marked by hemodynamic instability due to massive upper GI bleeding, through diagnosis and management. This highlights the crucial need for alert identification and prompt intervention.
Case Description/Methods: A 97-year-old female patient arrived at the Emergency Department (ED) with three occurrences of melena and one coffee-ground emesis accompanied by dizziness and light-headedness. A year prior, she was hospitalized for severe symptomatic anemia. An Esophagogastroduodenoscopy (EGD) revealed a large hiatal hernia with non-bleeding superficial gastric ulcers and erosions, identified as the bleeding source. In the ED, she was hypotensive and tachycardic with an initial hemoglobin level of 8.3 g/dL, later dropping to 6.6 g/dL. Melena was confirmed through digital rectal examination. A computed tomography (CT) scan revealed a large sliding hiatal hernia with most of the the stomach's content above the gastroesophageal junction.
Management involved intravenous fluid hydration and two units of packed red blood cells transfusion, raising her hemoglobin to 9.6 g/dL and improving symptoms. Repeat EGD affirmed the presence of Cameron lesions. Despite no active bleeding, a multidisciplinary team evaluated the risks and benefits of surgery, deciding to defer due to her advanced age. She was prescribed pantoprazole, sucralfate, levothyroxine, and hydrochlorothiazide, with a plan to continue proton pump inhibitor therapy indefinitely.
Discussion: Cameron lesions, though rare, can trigger significant morbidity, particularly in older patients with sizable hiatal hernias. Accurate detection necessitates vigilance and a detailed endoscopic examination. Treatment ranges from medical therapy to surgery, based on symptom severity and recurrence. This report underscores the importance of correctly identifying Cameron lesions via symptoms and crafting personalized management plans. These strategies should consider the patient's general health, bleeding intensity, and the potential surgical risks and benefits involved.

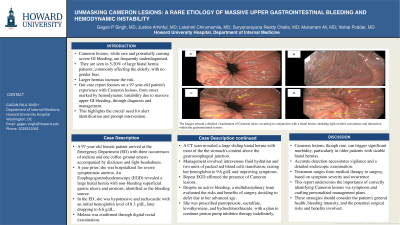
Figure: The Images present a detailed visualization of Cameron ulcers occurring in conjunction with a hiatal hernia, shedding light on their coexistence and interaction within the gastrointestinal system.
Disclosures:
Gagan Singh indicated no relevant financial relationships.
Justice Arhinful indicated no relevant financial relationships.
Lakshmi Chirumamilla indicated no relevant financial relationships.
Suryanarayana Reddy Challa indicated no relevant financial relationships.
Mukarram Jamat Ali indicated no relevant financial relationships.
Vishal Poddar indicated no relevant financial relationships.
Gagan P. Singh, MD1, Justice Arhinful, MD2, Lakshmi Chirumamilla, MD1, Suryanarayana Reddy Challa, MD1, Mukarram Jamat Ali, MD1, Vishal Poddar, MD1. P2053 - Unmasking Cameron Lesions: A Rare Etiology of Massive Upper Gastrointestinal Bleeding and Hemodynamic Instability, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

