Monday Poster Session
Category: GI Bleeding
P2060 - An Invading Stent: A Unique Case of Biliary Stent Impaction in the Cecum Causing Massive Rectal Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH1, Shady Geris, DO1, Mohita Jariwala, BA2, Mansi Patel, BS2, Mohamed Elagami, MD1, Ruhin Yuridullah, MD1
1St. Joseph's University Medical Center, Paterson, NJ; 2Rowan University School of Osteopathic Medicine, Paterson, NJ
Introduction: Endoscopic biliary stenting is a well-established intervention for treating biliary, hepatic, and pancreatic disorders. In this case, we describe an extremely rare event of acute bilio-cecal stent migration presenting as rectal bleeding.
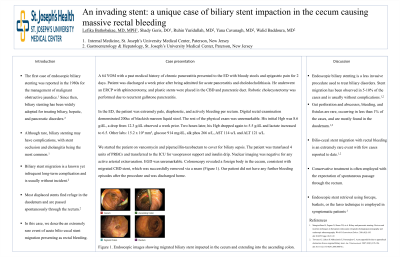
Case Description/Methods: A 64-year-old male with a history of chronic pancreatitis presented to the ED with bloody stools and epigastric pain for 2 days. Patient was recently discharged (a week ago) after being admitted for acute pancreatitis and choledocholithiasis. He underwent an ERCP with sphincterotomy, and plastic stents were placed in the CBD and pancreatic duct. Robotic cholecystectomy was performed due to recurrent gallstone pancreatitis. In the ED, the patient was extremely pale, diaphoretic, and actively bleeding per rectum. Digital rectal examination demonstrated 200 cc of blackish-maroon liquid stool. The rest of the physical exam was unremarkable. His initial Hgb was 8.6 g/dL, a drop from 12.3 g/dL observed a week prior. Two hours later, his Hgb dropped again to 5.5 g/dL and lactate increased to 6.5. Other labs: 15.2 x 103 mm3, glucose 914 mg/dL, alk phos 266 u/L, AST 114 u/L and ALT 121 u/L. We started the patient on vancomycin and piperacillin-tazobactam to cover for biliary sepsis. The patient was transfused 4 units of PRBCs and transferred to the ICU for vasopressor support and insulin drip. Nuclear imaging was negative for any active arterial extravasation. EGD was unremarkable. Colonoscopy revealed a foreign body in the cecum, consistent with migrated CBD stent, which was successfully removed via a snare. Our patient did not have any further bleeding episodes after the procedure and was discharged home.
Discussion: Endoscopic biliary stenting is a less invasive procedure used to treat biliary disorders. Stent migration has been observed in 5-10% of cases, usually without complications. Gut perforation and abscesses, bleeding, and fistulas are rare, occurring in less than 1% of the cases, and are mostly found in the duodenum. Bilio-cecal stent migration with rectal bleeding is an extremely rare event, with few cases reported to date. Co-existing bowel pathology predisposes patients to intestinal perforation as they impede the stent migration through the gut. Conservative treatment is often employed with the expectation of spontaneous passage through the rectum. Endoscopic stent retrieval using forceps, baskets, or the lasso technique is employed in symptomatic patients.

Disclosures:
Lefika Bathobakae, MD, MPH1, Shady Geris, DO1, Mohita Jariwala, BA2, Mansi Patel, BS2, Mohamed Elagami, MD1, Ruhin Yuridullah, MD1. P2060 - An Invading Stent: A Unique Case of Biliary Stent Impaction in the Cecum Causing Massive Rectal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. Joseph's University Medical Center, Paterson, NJ; 2Rowan University School of Osteopathic Medicine, Paterson, NJ
Introduction: Endoscopic biliary stenting is a well-established intervention for treating biliary, hepatic, and pancreatic disorders. In this case, we describe an extremely rare event of acute bilio-cecal stent migration presenting as rectal bleeding.
Case Description/Methods: A 64-year-old male with a history of chronic pancreatitis presented to the ED with bloody stools and epigastric pain for 2 days. Patient was recently discharged (a week ago) after being admitted for acute pancreatitis and choledocholithiasis. He underwent an ERCP with sphincterotomy, and plastic stents were placed in the CBD and pancreatic duct. Robotic cholecystectomy was performed due to recurrent gallstone pancreatitis. In the ED, the patient was extremely pale, diaphoretic, and actively bleeding per rectum. Digital rectal examination demonstrated 200 cc of blackish-maroon liquid stool. The rest of the physical exam was unremarkable. His initial Hgb was 8.6 g/dL, a drop from 12.3 g/dL observed a week prior. Two hours later, his Hgb dropped again to 5.5 g/dL and lactate increased to 6.5. Other labs: 15.2 x 103 mm3, glucose 914 mg/dL, alk phos 266 u/L, AST 114 u/L and ALT 121 u/L. We started the patient on vancomycin and piperacillin-tazobactam to cover for biliary sepsis. The patient was transfused 4 units of PRBCs and transferred to the ICU for vasopressor support and insulin drip. Nuclear imaging was negative for any active arterial extravasation. EGD was unremarkable. Colonoscopy revealed a foreign body in the cecum, consistent with migrated CBD stent, which was successfully removed via a snare. Our patient did not have any further bleeding episodes after the procedure and was discharged home.
Discussion: Endoscopic biliary stenting is a less invasive procedure used to treat biliary disorders. Stent migration has been observed in 5-10% of cases, usually without complications. Gut perforation and abscesses, bleeding, and fistulas are rare, occurring in less than 1% of the cases, and are mostly found in the duodenum. Bilio-cecal stent migration with rectal bleeding is an extremely rare event, with few cases reported to date. Co-existing bowel pathology predisposes patients to intestinal perforation as they impede the stent migration through the gut. Conservative treatment is often employed with the expectation of spontaneous passage through the rectum. Endoscopic stent retrieval using forceps, baskets, or the lasso technique is employed in symptomatic patients.

Figure: Figure 1. Endoscopic images showing migrated biliary stent impacted in the cecum and extending into the ascending colon.
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Shady Geris indicated no relevant financial relationships.
Mohita Jariwala indicated no relevant financial relationships.
Mansi Patel indicated no relevant financial relationships.
Mohamed Elagami indicated no relevant financial relationships.
Ruhin Yuridullah indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH1, Shady Geris, DO1, Mohita Jariwala, BA2, Mansi Patel, BS2, Mohamed Elagami, MD1, Ruhin Yuridullah, MD1. P2060 - An Invading Stent: A Unique Case of Biliary Stent Impaction in the Cecum Causing Massive Rectal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
