Monday Poster Session
Category: GI Bleeding
P2061 - Sinistral Portal Hypertension Due to a Pancreatic Pseudocyst: A Rare Cause of Upper GI Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Lefika Bathobakae, MD, MPH
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Lefika Bathobakae, MD, MPH, Sacide S. Ozgur, MD, Arielle Aiken, MD, Anas Mahmoud, MD, Ruhin Yuridullah, MD, Hardikkumar Shah, MD, MPH
St. Joseph's University Medical Center, Paterson, NJ
Introduction: Sinistral portal hypertension (SPH) is an infrequent complication of pancreatic disorders and an extremely rare cause of upper gastrointestinal bleeding (UGIB). SPH is the increase in portal venous pressure in patients with no cirrhosis. We report a rare case of massive hematemesis as a complication of pancreatic pseudocyst-induced SPH.
Case Description/Methods: A 45-year-old male with a history of chronic pancreatitis and pancreatic pseudocyst status post EUS with AXIOS stent placement presented to the ED after a syncopal episode. Before fainting, the patient reported sharp abdominal pain and nausea, but denied chest pain, palpitations, or diaphoresis. In the ED, vital signs were within normal ranges. Initial labs notable for Hgb 6.8 g/dL, and the patient was transfused 2 units of PRBCs. CT angiography of the abdomen and pelvis showed splenomegaly, splenic vein thrombosis, and a gastro-cystostomy tube with a large pseudocyst with debris. The next morning, a rapid response team was called for multiple episodes of hematemesis. EGD revealed blood clots in the gastric fundus and Type 1 isolated non-bleeding gastric varices. Because of worsening abdominal pain and recurrent episodes of acute blood loss, a splenectomy was performed. Patient received appropriate vaccines and underwent open splenectomy, distal pancreatectomy and pseudocyst resection, partial gastric resection, and repair of the gastrotomy. The patient was discharged on post-op day 10 with plans for at least one year of penicillin prophylaxis following splenectomy. He will also require booster doses of the vaccines.
Discussion:
SPH is an extremely rare clinical entity characterized by elevated splenoportal pressure due to splenic vein thrombosis (SVT). Unlike conventional portal hypertension, SPH presents with a patent-extrahepatic portal vein and normal liver function and is commonly associated with pancreatic disorders. Pancreatic pseudocysts can compress the splenic vein causing backflow of blood into the short gastric and gastroepiploic veins. SPH, very rarely, may cause UGIB due to isolated gastric varices, as was the case with our patient. Symptomatic SPH is a medical emergency requiring urgent surgical intervention. Splenectomy with surgical resection of the pancreatic mass is curative and decreases the inflow of blood into the splenoportal system. Patients with asplenia are at risk of post-infarction syndrome and post-splenectomy sepsis syndrome.

Disclosures:
Lefika Bathobakae, MD, MPH, Sacide S. Ozgur, MD, Arielle Aiken, MD, Anas Mahmoud, MD, Ruhin Yuridullah, MD, Hardikkumar Shah, MD, MPH. P2061 - Sinistral Portal Hypertension Due to a Pancreatic Pseudocyst: A Rare Cause of Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
St. Joseph's University Medical Center, Paterson, NJ
Introduction: Sinistral portal hypertension (SPH) is an infrequent complication of pancreatic disorders and an extremely rare cause of upper gastrointestinal bleeding (UGIB). SPH is the increase in portal venous pressure in patients with no cirrhosis. We report a rare case of massive hematemesis as a complication of pancreatic pseudocyst-induced SPH.
Case Description/Methods: A 45-year-old male with a history of chronic pancreatitis and pancreatic pseudocyst status post EUS with AXIOS stent placement presented to the ED after a syncopal episode. Before fainting, the patient reported sharp abdominal pain and nausea, but denied chest pain, palpitations, or diaphoresis. In the ED, vital signs were within normal ranges. Initial labs notable for Hgb 6.8 g/dL, and the patient was transfused 2 units of PRBCs. CT angiography of the abdomen and pelvis showed splenomegaly, splenic vein thrombosis, and a gastro-cystostomy tube with a large pseudocyst with debris. The next morning, a rapid response team was called for multiple episodes of hematemesis. EGD revealed blood clots in the gastric fundus and Type 1 isolated non-bleeding gastric varices. Because of worsening abdominal pain and recurrent episodes of acute blood loss, a splenectomy was performed. Patient received appropriate vaccines and underwent open splenectomy, distal pancreatectomy and pseudocyst resection, partial gastric resection, and repair of the gastrotomy. The patient was discharged on post-op day 10 with plans for at least one year of penicillin prophylaxis following splenectomy. He will also require booster doses of the vaccines.
Discussion:
SPH is an extremely rare clinical entity characterized by elevated splenoportal pressure due to splenic vein thrombosis (SVT). Unlike conventional portal hypertension, SPH presents with a patent-extrahepatic portal vein and normal liver function and is commonly associated with pancreatic disorders. Pancreatic pseudocysts can compress the splenic vein causing backflow of blood into the short gastric and gastroepiploic veins. SPH, very rarely, may cause UGIB due to isolated gastric varices, as was the case with our patient. Symptomatic SPH is a medical emergency requiring urgent surgical intervention. Splenectomy with surgical resection of the pancreatic mass is curative and decreases the inflow of blood into the splenoportal system. Patients with asplenia are at risk of post-infarction syndrome and post-splenectomy sepsis syndrome.

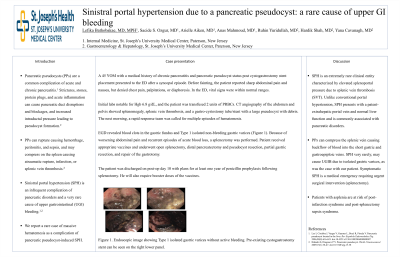
Figure: Figure 1. Endoscopic view: Type 1 isolated gastric varices without active bleeding. Old blood and blood clots in the gastric fundus and the gastric body.
Disclosures:
Lefika Bathobakae indicated no relevant financial relationships.
Sacide Ozgur indicated no relevant financial relationships.
Arielle Aiken indicated no relevant financial relationships.
Anas Mahmoud indicated no relevant financial relationships.
Ruhin Yuridullah indicated no relevant financial relationships.
Hardikkumar Shah indicated no relevant financial relationships.
Lefika Bathobakae, MD, MPH, Sacide S. Ozgur, MD, Arielle Aiken, MD, Anas Mahmoud, MD, Ruhin Yuridullah, MD, Hardikkumar Shah, MD, MPH. P2061 - Sinistral Portal Hypertension Due to a Pancreatic Pseudocyst: A Rare Cause of Upper GI Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
