Monday Poster Session
Category: GI Bleeding
P2062 - Gastrointestinal Ulceration as a Manifestation of Severe Dermatomyositis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall

Dhanushya Battepati, MD, MS
Baylor Scott & White Health
Temple, TX
Presenting Author(s)
Daniel O'Shea, MD1, Dhanushya Battepati, MD, MS2, Brandon Speedy, MD3, Benjamin Hart, MD, PhD4
1West Virginia University, Morgantown, WV; 2Baylor Scott & White Health, Temple, TX; 3Madigan Army Medical Center, Tacoma, WA; 4University of Michigan, Ann Arbor, MI
Introduction: A 32-year-old female with a history of adult-onset dermatomyositis presented to the emergency department with symptoms of fever and altered mental status. The patient was admitted for septic shock and multi-organismal pneumonia.
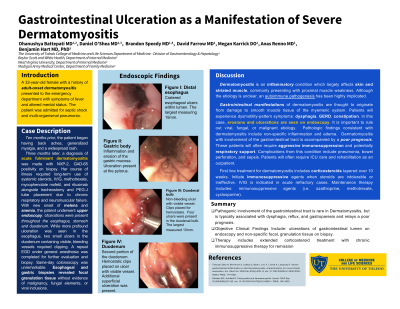
Case Description/Methods: Ten months prior, the patient began having back aches, generalized myalgia, and widespread rash. A diagnosis of acute fulminant dermatomyositis was made upon biopsy, showing both NXP-2 and GAD-65 positivity. To this point, her course of illness required long-term use of systemic steroids, IVIG, multiple immunosuppressive drugs, and tracheostomy placement due to chronic respiratory and neuromuscular failure. Onset of melena and anemia this admission prompted upper endoscopy. Ulcerations were present throughout the esophagus, stomach, and duodenum. While more profound ulceration was seen in the esophagus, two small ulcers in the duodenum containing visible, bleeding vessels required clipping. A repeat EGD under general anesthesia was completed for further evaluation and biopsy. Same-day colonoscopy was unremarkable. Esophageal and gastric biopsies revealed focal granulation tissue without evidence of malignancy, fungal elements, or viral inclusions.
Discussion: Dermatomyositis is an inflammatory condition which largely affects skin and striated muscle, commonly presenting with proximal muscle weakness. Although the etiology is unclear, autoimmune pathogenesis has been highly implicated. Gastrointestinal manifestations of dermatomyositis are thought to originate from damage to smooth muscle tissue of the myenteric system. Patients may experience dysmotility-pattern symptoms: dysphagia, GERD, constipation. In this case, erosions and ulcerations are seen on endoscopy. It is important to rule out viral, fungal, or malignant etiology with biopsy. Pathologic findings consistent with dermatomyositis include non-specific inflammation and edema. Dermatomyositis with gastrointestinal involvement portends a poor prognosis. These patients often require aggressive immunosuppression and potentially respiratory support. Complications include pneumonia, bowel perforation, and sepsis. Patients will often require ICU care and long-term rehabilitation. Dermatomyositis treatment includes corticosteroids tapered over 10 weeks. Immunosuppressive agents can be used when steroids are intolerable or ineffective. IVIG is indicated in acute refractory cases. Maintenance therapy includes immunosuppressive agents like azathioprine or methotrexate.
Disclosures:
Daniel O'Shea, MD1, Dhanushya Battepati, MD, MS2, Brandon Speedy, MD3, Benjamin Hart, MD, PhD4. P2062 - Gastrointestinal Ulceration as a Manifestation of Severe Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1West Virginia University, Morgantown, WV; 2Baylor Scott & White Health, Temple, TX; 3Madigan Army Medical Center, Tacoma, WA; 4University of Michigan, Ann Arbor, MI
Introduction: A 32-year-old female with a history of adult-onset dermatomyositis presented to the emergency department with symptoms of fever and altered mental status. The patient was admitted for septic shock and multi-organismal pneumonia.
Case Description/Methods: Ten months prior, the patient began having back aches, generalized myalgia, and widespread rash. A diagnosis of acute fulminant dermatomyositis was made upon biopsy, showing both NXP-2 and GAD-65 positivity. To this point, her course of illness required long-term use of systemic steroids, IVIG, multiple immunosuppressive drugs, and tracheostomy placement due to chronic respiratory and neuromuscular failure. Onset of melena and anemia this admission prompted upper endoscopy. Ulcerations were present throughout the esophagus, stomach, and duodenum. While more profound ulceration was seen in the esophagus, two small ulcers in the duodenum containing visible, bleeding vessels required clipping. A repeat EGD under general anesthesia was completed for further evaluation and biopsy. Same-day colonoscopy was unremarkable. Esophageal and gastric biopsies revealed focal granulation tissue without evidence of malignancy, fungal elements, or viral inclusions.
Discussion: Dermatomyositis is an inflammatory condition which largely affects skin and striated muscle, commonly presenting with proximal muscle weakness. Although the etiology is unclear, autoimmune pathogenesis has been highly implicated. Gastrointestinal manifestations of dermatomyositis are thought to originate from damage to smooth muscle tissue of the myenteric system. Patients may experience dysmotility-pattern symptoms: dysphagia, GERD, constipation. In this case, erosions and ulcerations are seen on endoscopy. It is important to rule out viral, fungal, or malignant etiology with biopsy. Pathologic findings consistent with dermatomyositis include non-specific inflammation and edema. Dermatomyositis with gastrointestinal involvement portends a poor prognosis. These patients often require aggressive immunosuppression and potentially respiratory support. Complications include pneumonia, bowel perforation, and sepsis. Patients will often require ICU care and long-term rehabilitation. Dermatomyositis treatment includes corticosteroids tapered over 10 weeks. Immunosuppressive agents can be used when steroids are intolerable or ineffective. IVIG is indicated in acute refractory cases. Maintenance therapy includes immunosuppressive agents like azathioprine or methotrexate.
Disclosures:
Daniel O'Shea indicated no relevant financial relationships.
Dhanushya Battepati indicated no relevant financial relationships.
Brandon Speedy indicated no relevant financial relationships.
Benjamin Hart indicated no relevant financial relationships.
Daniel O'Shea, MD1, Dhanushya Battepati, MD, MS2, Brandon Speedy, MD3, Benjamin Hart, MD, PhD4. P2062 - Gastrointestinal Ulceration as a Manifestation of Severe Dermatomyositis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

