Monday Poster Session
Category: GI Bleeding
P2068 - Choledochojejunal Varices in a Post-Whipple Patient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Sara Gottesman, MD
Dell Medical School at The University of Texas at Austin
Austin, TX
Presenting Author(s)
Sara Gottesman, MD1, Nikitha Gangasani, MD1, Sagarika Satyavada, MD2
1Dell Medical School at The University of Texas at Austin, Austin, TX; 2Dell Medical School, Austin, TX
Introduction: Ectopic varices represent 5% of all variceal bleeding but have mortality nearing 40% due to difficulty in diagnosis and treatment. Herein, we present a case of bleeding choledochojejunal (CDJ) varices in a patient with cirrhosis and altered surgical anatomy. Our case adds to the small but growing literature of successful endoscopic intervention for ectopic variceal bleeding.
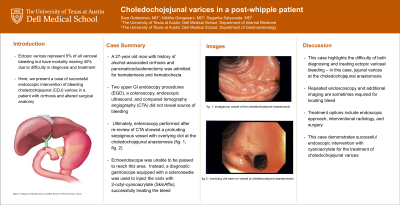
Case Description/Methods: A 27-year old man with alcohol-associated cirrhosis and pancreaticoduodenectomy due to trauma from prior abdominal gunshot wound was admitted for hematemesis and hematochezia. Initial upper GI Endoscopy (EGD) revealed esophageal varices, a normal gastro-jejunal anastomosis, and a gastric protuberance which was thought to be a gastric varix; none had stigmata of recent bleeding. A colonoscopy showed copious blood in the colon into the terminal ileum. Computed tomography angiography (CTA) of his abdomen demonstrated chronic portal venous thrombosis (PVT), but no active bleed. An EGD was repeated and showed a large amount of blood in the stomach and afferent limb; again, no source was identified. Endoscopic ultrasound (EUS) was also performed which showed that the gastric protuberance was extra-luminal compression by large splenic varices rather than gastric varices. Given ongoing bleeding, the CTA was re-examined, which demonstrated enlarged jejunal vessels along the afferent (pancreatobiliary) limb. Thus, enteroscopy was performed which revealed a protruding serpiginous vessel with overlying clot at the choledochojejunal anastomosis (fig. A, fig. B). Passage of echoendoscope was attempted to treat the choledochojejunal varices under EUS guidance but was unable to reach this area. A diagnostic gastroscope equipped with a scleroneedle was used to inject the varix with 2-octyl-cyanoacrylate (SkinAffix). The patient remained hemodynamically stable without further episodes of bleeding.
Discussion: This case highlights the difficulty of both diagnosing and treating ectopic variceal bleeding – in our case, jejunal varices at the CDJ anastomosis. Our patient had several predisposing factors, including portal hypertension, continued alcohol use, PVT, and possible adhesions from surgery. Treatment options include endoscopy, interventional radiology (IR) and surgery. His PVT precluded IR intervention, and his advanced liver disease precluded him from surgical options. In summary, this case demonstrates successful endoscopic intervention with cyanoacrylate for the treatment of choledochojejunal varices.

Disclosures:
Sara Gottesman, MD1, Nikitha Gangasani, MD1, Sagarika Satyavada, MD2. P2068 - Choledochojejunal Varices in a Post-Whipple Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Dell Medical School at The University of Texas at Austin, Austin, TX; 2Dell Medical School, Austin, TX
Introduction: Ectopic varices represent 5% of all variceal bleeding but have mortality nearing 40% due to difficulty in diagnosis and treatment. Herein, we present a case of bleeding choledochojejunal (CDJ) varices in a patient with cirrhosis and altered surgical anatomy. Our case adds to the small but growing literature of successful endoscopic intervention for ectopic variceal bleeding.
Case Description/Methods: A 27-year old man with alcohol-associated cirrhosis and pancreaticoduodenectomy due to trauma from prior abdominal gunshot wound was admitted for hematemesis and hematochezia. Initial upper GI Endoscopy (EGD) revealed esophageal varices, a normal gastro-jejunal anastomosis, and a gastric protuberance which was thought to be a gastric varix; none had stigmata of recent bleeding. A colonoscopy showed copious blood in the colon into the terminal ileum. Computed tomography angiography (CTA) of his abdomen demonstrated chronic portal venous thrombosis (PVT), but no active bleed. An EGD was repeated and showed a large amount of blood in the stomach and afferent limb; again, no source was identified. Endoscopic ultrasound (EUS) was also performed which showed that the gastric protuberance was extra-luminal compression by large splenic varices rather than gastric varices. Given ongoing bleeding, the CTA was re-examined, which demonstrated enlarged jejunal vessels along the afferent (pancreatobiliary) limb. Thus, enteroscopy was performed which revealed a protruding serpiginous vessel with overlying clot at the choledochojejunal anastomosis (fig. A, fig. B). Passage of echoendoscope was attempted to treat the choledochojejunal varices under EUS guidance but was unable to reach this area. A diagnostic gastroscope equipped with a scleroneedle was used to inject the varix with 2-octyl-cyanoacrylate (SkinAffix). The patient remained hemodynamically stable without further episodes of bleeding.
Discussion: This case highlights the difficulty of both diagnosing and treating ectopic variceal bleeding – in our case, jejunal varices at the CDJ anastomosis. Our patient had several predisposing factors, including portal hypertension, continued alcohol use, PVT, and possible adhesions from surgery. Treatment options include endoscopy, interventional radiology (IR) and surgery. His PVT precluded IR intervention, and his advanced liver disease precluded him from surgical options. In summary, this case demonstrates successful endoscopic intervention with cyanoacrylate for the treatment of choledochojejunal varices.

Figure: Figures A and B: protruding serpiginous vessel with overlying clot at the choledochojejunal anastomosis
Disclosures:
Sara Gottesman indicated no relevant financial relationships.
Nikitha Gangasani indicated no relevant financial relationships.
Sagarika Satyavada indicated no relevant financial relationships.
Sara Gottesman, MD1, Nikitha Gangasani, MD1, Sagarika Satyavada, MD2. P2068 - Choledochojejunal Varices in a Post-Whipple Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
