Monday Poster Session
Category: GI Bleeding
P2069 - Duodenal Gastrointestinal Stromal Tumor
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- PP
Preethika Palani, MD
Trinity Health Ann Arbor Hospital
Ypsilanti, MI
Presenting Author(s)
Preethika Palani, MD1, Ann Saliares, DO2, Naresh T. Gunaratnam, MD3
1Trinity Health Ann Arbor Hospital, Ypsilanti, MI; 2St. Joseph Mercy Ann Arbor Hospital, Ypsilanti, MI; 3Huron Gastroenterology, Ypsilanti, MI
Introduction: A gastrointestinal stromal tumor (GIST) is a rare pathology accounting for only 1% to 3% of all gastrointestinal tumors; however, they are the most common mesenchymal neoplasms of the GI tract. They originate from the interstitial cells of Cajal. They typically originate in the stomach (50% to 75%) or the small bowel (20%), less frequently in the colon and rectum. GISTs are predominantly in older adults between 55-60 years old. Our case details an elderly patient presenting with recurrent bleeding due to a duodenal GIST.
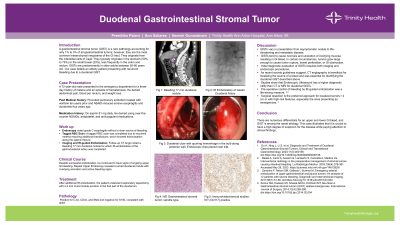
Case Description/Methods: A 72-year-old male presented to the ER for a three-day history of melena and hematemesis. He denied abdominal pain, blood per rectum, and weight loss. Past medical history was significant for provoked pulmonary embolism and NSAID-induced erosive esophagitis and duodenitis. Endoscopy noted grade C esophagitis without a clear source of bleeding. Due to recurrent melena requiring additional transfusions, a tagged RBC scan was completed, which showed extravasation along the splenic flexure. Follow-up CT Angio noted a bleeding 17 mm duodenal nodule for which IR-embolization of the gastroduodenal artery was completed. Despite successful embolization, he continued to have signs of ongoing upper GI bleeding. Repeat Upper Endoscopy revealed a small duodenal nodule with overlying ulceration and active bleeding signs. After additional IR embolization, the patient underwent exploratory laparotomy with a 2 mm mural nodule excision in the first part of the duodenum. Pathology was positive for C-kit, CD34, and SMA and negative for S100, consistent with GIST.
Discussion: GISTs vary in presentation from asymptomatic nodule to life-threatening and metastatic disease. GISTs tend to cause necrosis and ulceration of overlying mucosa resulting in GI bleed. In certain circumstances, tumors grow large enough to cause tumor rupture, bowel perforation, or GI obstruction. Initial diagnostic evaluation of GISTs requires both imaging and endoscopic procedures. As recent society guidelines suggest, CT angiography is beneficial for localizing the source of a bleed and was essential for identifying the duodenal GIST described above. Studies show that Endoscopic Ultrasound has a higher diagnostic utility than CT or MRI for duodenal GISTs. Pre-operative control of bleeding by IR-guided embolization was a life-saving measure. Surgical resection is the preferred approach for localized tumors > 2 cm or with high-risk features, especially the ones presenting as emergencies.
Disclosures:
Preethika Palani, MD1, Ann Saliares, DO2, Naresh T. Gunaratnam, MD3. P2069 - Duodenal Gastrointestinal Stromal Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Trinity Health Ann Arbor Hospital, Ypsilanti, MI; 2St. Joseph Mercy Ann Arbor Hospital, Ypsilanti, MI; 3Huron Gastroenterology, Ypsilanti, MI
Introduction: A gastrointestinal stromal tumor (GIST) is a rare pathology accounting for only 1% to 3% of all gastrointestinal tumors; however, they are the most common mesenchymal neoplasms of the GI tract. They originate from the interstitial cells of Cajal. They typically originate in the stomach (50% to 75%) or the small bowel (20%), less frequently in the colon and rectum. GISTs are predominantly in older adults between 55-60 years old. Our case details an elderly patient presenting with recurrent bleeding due to a duodenal GIST.
Case Description/Methods: A 72-year-old male presented to the ER for a three-day history of melena and hematemesis. He denied abdominal pain, blood per rectum, and weight loss. Past medical history was significant for provoked pulmonary embolism and NSAID-induced erosive esophagitis and duodenitis. Endoscopy noted grade C esophagitis without a clear source of bleeding. Due to recurrent melena requiring additional transfusions, a tagged RBC scan was completed, which showed extravasation along the splenic flexure. Follow-up CT Angio noted a bleeding 17 mm duodenal nodule for which IR-embolization of the gastroduodenal artery was completed. Despite successful embolization, he continued to have signs of ongoing upper GI bleeding. Repeat Upper Endoscopy revealed a small duodenal nodule with overlying ulceration and active bleeding signs. After additional IR embolization, the patient underwent exploratory laparotomy with a 2 mm mural nodule excision in the first part of the duodenum. Pathology was positive for C-kit, CD34, and SMA and negative for S100, consistent with GIST.
Discussion: GISTs vary in presentation from asymptomatic nodule to life-threatening and metastatic disease. GISTs tend to cause necrosis and ulceration of overlying mucosa resulting in GI bleed. In certain circumstances, tumors grow large enough to cause tumor rupture, bowel perforation, or GI obstruction. Initial diagnostic evaluation of GISTs requires both imaging and endoscopic procedures. As recent society guidelines suggest, CT angiography is beneficial for localizing the source of a bleed and was essential for identifying the duodenal GIST described above. Studies show that Endoscopic Ultrasound has a higher diagnostic utility than CT or MRI for duodenal GISTs. Pre-operative control of bleeding by IR-guided embolization was a life-saving measure. Surgical resection is the preferred approach for localized tumors > 2 cm or with high-risk features, especially the ones presenting as emergencies.
Disclosures:
Preethika Palani indicated no relevant financial relationships.
Ann Saliares indicated no relevant financial relationships.
Naresh Gunaratnam indicated no relevant financial relationships.
Preethika Palani, MD1, Ann Saliares, DO2, Naresh T. Gunaratnam, MD3. P2069 - Duodenal Gastrointestinal Stromal Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
