Monday Poster Session
Category: GI Bleeding
P2073 - Small Bowel Metastasis of Melanoma Presenting as Overt Gastrointestinal Bleeding
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- PA
Prince Addo Ameyaw, MD
Bridgeport Hospital/Yale New Haven Health
BRIDGEORT, CT
Presenting Author(s)
PRINCE A. AMEYAW, MD1, Cheng-Hung Tai, MD2, Karthik Mathialagan, MD2, Pietro Andres, MD3
1Bridgeport Hospital/Yale New Haven Health, Bridgeport, CT; 2Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 3Bridgeport Hospital/Yale New Haven Health, Stratford, CT
Introduction: Melanoma has a predilection for metastasis to the gastrointestinal tract and accounts for about 1-3% of intestinal tumors. Overt GI bleeding as a presentation of small bowel metastasis is rare. We report a case of metastatic melanoma (MM) presenting as GI bleeding.
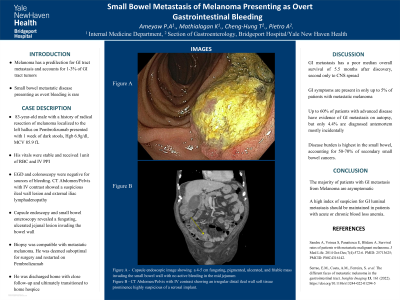
Case Description/Methods: An 83-year-old man with a history of melanoma localized to the left hallux treated with radical resection complicated by pulmonary metastasis and pulmonary embolism on low molecular weight heparin (LMWH) and Pembrolizumab, presented to the ED with a 1-week history of dark stools and generalized weakness. Initial vitals: BP 119/86, HR 89, SPO2 of 98% on room air. His abdominal examination was unremarkable. Labs were significant for Hgb 6.6 g/dl, MCV 85.9fL, and elevated alkaline phosphatase 160U/L. LMWH was held and patient was started on intravenous proton pump inhibitor therapy and given one unit of packed red blood cells. Upper GI endoscopy and subsequent colonoscopy were negative for sources of bleeding. CT abdomen and pelvis with IV contrast showed an irregular distal ileal wall soft tissue prominence highly suspicious of a serosal implant and an 8 cm left external iliac node but no hepatic lesions. Capsule endoscopy and small bowel enteroscopy showed a 4-5 cm fungating, pigmented, ulcerated and friable mass invading the small bowel wall with no active bleeding in the mid jejunum. The lesion was biopsied, and hemostasis was achieved via epinephrine injection and hemostatic clips. Histopathologic examination of the jejunal lesion was compatible with MM. He was deemed suboptimal for surgery and restarted on Pembrolizumab. Patient was subsequently discharged home with close follow-up for blood transfusions as needed. Patient was ultimately transitioned to home hospice.
Discussion: GI symptoms such as obstruction, bleeding and abdominal pain are seen in about 2-5% of patients with metastatic melanoma. The majority of GI spread is diagnosed incidentally. Up to 60% of patients with advanced disease have evidence of GI metastasis on autopsy, but only 4.4% are diagnosed antemortem. Disease burden is highest in the small bowel, accounting for 50-70% of secondary small bowel cancers. GI metastasis has a poor median overall survival of 5.5 months after discovery, second only to CNS spread. Given that majority of GI spread is asymptomatic and associated with a grim prognosis, a high index of suspicion for GI luminal metastasis should be maintained in patients with acute or chronic blood loss anemia.

Disclosures:
PRINCE A. AMEYAW, MD1, Cheng-Hung Tai, MD2, Karthik Mathialagan, MD2, Pietro Andres, MD3. P2073 - Small Bowel Metastasis of Melanoma Presenting as Overt Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Bridgeport Hospital/Yale New Haven Health, Bridgeport, CT; 2Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 3Bridgeport Hospital/Yale New Haven Health, Stratford, CT
Introduction: Melanoma has a predilection for metastasis to the gastrointestinal tract and accounts for about 1-3% of intestinal tumors. Overt GI bleeding as a presentation of small bowel metastasis is rare. We report a case of metastatic melanoma (MM) presenting as GI bleeding.
Case Description/Methods: An 83-year-old man with a history of melanoma localized to the left hallux treated with radical resection complicated by pulmonary metastasis and pulmonary embolism on low molecular weight heparin (LMWH) and Pembrolizumab, presented to the ED with a 1-week history of dark stools and generalized weakness. Initial vitals: BP 119/86, HR 89, SPO2 of 98% on room air. His abdominal examination was unremarkable. Labs were significant for Hgb 6.6 g/dl, MCV 85.9fL, and elevated alkaline phosphatase 160U/L. LMWH was held and patient was started on intravenous proton pump inhibitor therapy and given one unit of packed red blood cells. Upper GI endoscopy and subsequent colonoscopy were negative for sources of bleeding. CT abdomen and pelvis with IV contrast showed an irregular distal ileal wall soft tissue prominence highly suspicious of a serosal implant and an 8 cm left external iliac node but no hepatic lesions. Capsule endoscopy and small bowel enteroscopy showed a 4-5 cm fungating, pigmented, ulcerated and friable mass invading the small bowel wall with no active bleeding in the mid jejunum. The lesion was biopsied, and hemostasis was achieved via epinephrine injection and hemostatic clips. Histopathologic examination of the jejunal lesion was compatible with MM. He was deemed suboptimal for surgery and restarted on Pembrolizumab. Patient was subsequently discharged home with close follow-up for blood transfusions as needed. Patient was ultimately transitioned to home hospice.
Discussion: GI symptoms such as obstruction, bleeding and abdominal pain are seen in about 2-5% of patients with metastatic melanoma. The majority of GI spread is diagnosed incidentally. Up to 60% of patients with advanced disease have evidence of GI metastasis on autopsy, but only 4.4% are diagnosed antemortem. Disease burden is highest in the small bowel, accounting for 50-70% of secondary small bowel cancers. GI metastasis has a poor median overall survival of 5.5 months after discovery, second only to CNS spread. Given that majority of GI spread is asymptomatic and associated with a grim prognosis, a high index of suspicion for GI luminal metastasis should be maintained in patients with acute or chronic blood loss anemia.

Figure: A : CT Abdomen Pelvis with IV Contrast showing an irregular soft tissue prominence along the wall of distal Ileum highly suspicious of a serosal implant
B : Capsule Endoscopy image showing a fungating, pigmented and ulcerated mass invading the mid-jejunal wall
B : Capsule Endoscopy image showing a fungating, pigmented and ulcerated mass invading the mid-jejunal wall
Disclosures:
PRINCE AMEYAW indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Pietro Andres indicated no relevant financial relationships.
PRINCE A. AMEYAW, MD1, Cheng-Hung Tai, MD2, Karthik Mathialagan, MD2, Pietro Andres, MD3. P2073 - Small Bowel Metastasis of Melanoma Presenting as Overt Gastrointestinal Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
