Monday Poster Session
Category: GI Bleeding
P2074 - A Case of Colonic Perforation Presenting With Lower Gastrointestinal Bleeding in Post-Cardiac Surgery Patient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Jiaxin Dong, MD
Qingdao University College of Medical Science
Qingdao, Shandong, China (People's Republic)
Presenting Author(s)
Jiaxin Dong, MD1, Vladislav Fomin, MD2, SriHari Mahadev, MD, MS3, Aiya Aboubakr, MD4, David Wan, BS, MD5
1Qingdao University College of Medical Science, New Haven, CT; 2New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 3New York-Presbyterian/Weill Cornell Medical Center, New York, NY; 4New York Presbyterian-Weill Cornell Medical Center, New York, NY; 5Weill Cornell Medicine, New York, NY
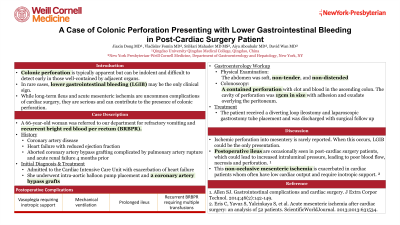
Introduction: Colonic perforation is typically apparent, but can be indolent and difficult to detect early in those well-contained by adjacent organs. In rare cases, lower gastrointestinal bleeding (LGIB) may be the only clinical sign. While long-term ileus and acute mesenteric ischemia are uncommon complications of cardiac surgery, they are serious and can contribute to the presence of colonic perforation.
Case Description/Methods: A 66-year-old woman was referred to our department for refractory vomiting and recurrent bright red blood per rectum (BRBPR). She had a significant medical history of coronary artery disease, status post 3 stent placements, heart failure with reduced ejection fraction, aborted coronary artery bypass grafting complicated by pulmonary artery rupture and acute renal failure 4 months prior. The patient was admitted to the hospital with exacerbation of heart failure and underwent intra-aortic balloon pump placement and 2 coronary artery bypass grafts. Her postoperative course was complicated by vasoplegia requiring inotropic support, mechanical ventilation, prolonged ileus and recurrent BRBPR requiring multiple transfusions. Physical examination, the abdomen was soft, non-tender, and non-distended. Bedside colonoscopy revealed heavy clot burden and a contained perforation with clot and blood in the ascending colon. The cavity of perforation was 15cm in size with adhesion and exudate overlying the peritoneum. The patient received a diverting loop ileostomy and laparoscopic gastrostomy tube placement and was discharged with surgical follow up.
Discussion: Colonic perforation is a rare cause of LGIB. Ischemic perforation is commonly seen in the left colon, but perforation into mesentery is rarely reported. When this occurs, the contents of colon, including the colonic bacterial flora, are prevented from being released and there is an absence of peritoneal signs, free air or fluid, especially in postoperative patients who are under sedation and ventilation. In some cases, LGIB could be the only presentation, and colonic perforation may be an incidental finding, as seen in this patient. Postoperative ileus are occasionally seen in post-cardiac surgery patients, which could lead to increased intraluminal pressure exceeding intestinal perfusion pressure, leading to poor blood flow, necrosis and perforation. This non-occlusive mesenteric ischemia is exacerbated in cardiac patients whom often have low cardiac output and require inotropic support.
Disclosures:
Jiaxin Dong, MD1, Vladislav Fomin, MD2, SriHari Mahadev, MD, MS3, Aiya Aboubakr, MD4, David Wan, BS, MD5. P2074 - A Case of Colonic Perforation Presenting With Lower Gastrointestinal Bleeding in Post-Cardiac Surgery Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Qingdao University College of Medical Science, New Haven, CT; 2New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 3New York-Presbyterian/Weill Cornell Medical Center, New York, NY; 4New York Presbyterian-Weill Cornell Medical Center, New York, NY; 5Weill Cornell Medicine, New York, NY
Introduction: Colonic perforation is typically apparent, but can be indolent and difficult to detect early in those well-contained by adjacent organs. In rare cases, lower gastrointestinal bleeding (LGIB) may be the only clinical sign. While long-term ileus and acute mesenteric ischemia are uncommon complications of cardiac surgery, they are serious and can contribute to the presence of colonic perforation.
Case Description/Methods: A 66-year-old woman was referred to our department for refractory vomiting and recurrent bright red blood per rectum (BRBPR). She had a significant medical history of coronary artery disease, status post 3 stent placements, heart failure with reduced ejection fraction, aborted coronary artery bypass grafting complicated by pulmonary artery rupture and acute renal failure 4 months prior. The patient was admitted to the hospital with exacerbation of heart failure and underwent intra-aortic balloon pump placement and 2 coronary artery bypass grafts. Her postoperative course was complicated by vasoplegia requiring inotropic support, mechanical ventilation, prolonged ileus and recurrent BRBPR requiring multiple transfusions. Physical examination, the abdomen was soft, non-tender, and non-distended. Bedside colonoscopy revealed heavy clot burden and a contained perforation with clot and blood in the ascending colon. The cavity of perforation was 15cm in size with adhesion and exudate overlying the peritoneum. The patient received a diverting loop ileostomy and laparoscopic gastrostomy tube placement and was discharged with surgical follow up.
Discussion: Colonic perforation is a rare cause of LGIB. Ischemic perforation is commonly seen in the left colon, but perforation into mesentery is rarely reported. When this occurs, the contents of colon, including the colonic bacterial flora, are prevented from being released and there is an absence of peritoneal signs, free air or fluid, especially in postoperative patients who are under sedation and ventilation. In some cases, LGIB could be the only presentation, and colonic perforation may be an incidental finding, as seen in this patient. Postoperative ileus are occasionally seen in post-cardiac surgery patients, which could lead to increased intraluminal pressure exceeding intestinal perfusion pressure, leading to poor blood flow, necrosis and perforation. This non-occlusive mesenteric ischemia is exacerbated in cardiac patients whom often have low cardiac output and require inotropic support.
Disclosures:
Jiaxin Dong indicated no relevant financial relationships.
Vladislav Fomin indicated no relevant financial relationships.
SriHari Mahadev: Boston Scientific – Consultant. Conmed – Consultant.
Aiya Aboubakr indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Jiaxin Dong, MD1, Vladislav Fomin, MD2, SriHari Mahadev, MD, MS3, Aiya Aboubakr, MD4, David Wan, BS, MD5. P2074 - A Case of Colonic Perforation Presenting With Lower Gastrointestinal Bleeding in Post-Cardiac Surgery Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
