Monday Poster Session
Category: GI Bleeding
P2075 - Dieulafoy Lesion Masquerading as a Gastric Varix: An Unexpected Finding on Upper Endoscopy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Alexander M. Carlson, DO
University at Buffalo
Buffalo, NY
Presenting Author(s)
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Elizabeth Z. Gregory, MD, Mayada Ismail, MD
University at Buffalo, Buffalo, NY
Introduction: Dieulafoy lesions are aberrant submucosal vessels that comprise about 1.5% of cases of upper gastrointestinal bleeding. They are an important consideration for every endoscopist, even in the face of conflicting evidence when varices overwhelmingly appear to be the diagnosis at hand. Here we present a unique case of a Dieulafoy lesion disguised as a gastric varix.
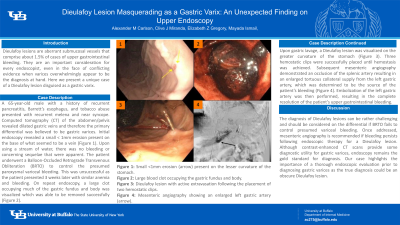
Case Description/Methods: A 65-year-old male with a history of recurrent pancreatitis, Barrett’s esophagus, and tobacco abuse presented with recurrent melena and near syncope. Computed tomography (CT) of the abdomen/pelvis revealed dilated gastric veins and therefore the primary differential was believed to be gastric varices. Initial endoscopy revealed a small < 1mm erosion present on the base of what seemed to be a vein (Figure 1). Upon using a stream of water, there was no bleeding or concerning sequelae that were apparent. The patient underwent a Balloon-Occluded Retrograde Transvenous Obliteration (BRTO) to control the presumed paroxysmal variceal bleeding. This was unsuccessful as the patient presented 3 weeks later with similar anemia and bleeding. On repeat endoscopy, a large clot occupying much of the gastric fundus and body was visualized which was able to be removed successfully (Figure 2). Upon gastric lavage, a Dieulafoy lesion was visualized on the greater curvature of the stomach (Figure 3). Three hemostatic clips were successfully placed until hemostasis was achieved. Subsequent mesenteric angiography demonstrated an occlusion of the splenic artery resulting in an enlarged tortuous collateral supply from the left gastric artery, which was determined to be the source of the patient’s bleeding (Figure 4). Embolization of the left gastric artery was then performed, resulting in the complete resolution of the patient’s upper gastrointestinal bleeding.
Discussion: The diagnosis of Dieulafoy lesions can be rather challenging and should be considered on the differential if BRTO fails to control presumed variceal bleeding. Once addressed, mesenteric angiography is recommended if bleeding persists following endoscopic therapy for a Dieulafoy lesion. Although contrast-enhanced CT scans provide some diagnostic utility for gastric varices, endoscopy remains the gold standard for diagnosis. Our case highlights the importance of a thorough endoscopic evaluation prior to diagnosing gastric varices as the true diagnosis could be an obscure Dieulafoy lesion.

Disclosures:
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Elizabeth Z. Gregory, MD, Mayada Ismail, MD. P2075 - Dieulafoy Lesion Masquerading as a Gastric Varix: An Unexpected Finding on Upper Endoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Dieulafoy lesions are aberrant submucosal vessels that comprise about 1.5% of cases of upper gastrointestinal bleeding. They are an important consideration for every endoscopist, even in the face of conflicting evidence when varices overwhelmingly appear to be the diagnosis at hand. Here we present a unique case of a Dieulafoy lesion disguised as a gastric varix.
Case Description/Methods: A 65-year-old male with a history of recurrent pancreatitis, Barrett’s esophagus, and tobacco abuse presented with recurrent melena and near syncope. Computed tomography (CT) of the abdomen/pelvis revealed dilated gastric veins and therefore the primary differential was believed to be gastric varices. Initial endoscopy revealed a small < 1mm erosion present on the base of what seemed to be a vein (Figure 1). Upon using a stream of water, there was no bleeding or concerning sequelae that were apparent. The patient underwent a Balloon-Occluded Retrograde Transvenous Obliteration (BRTO) to control the presumed paroxysmal variceal bleeding. This was unsuccessful as the patient presented 3 weeks later with similar anemia and bleeding. On repeat endoscopy, a large clot occupying much of the gastric fundus and body was visualized which was able to be removed successfully (Figure 2). Upon gastric lavage, a Dieulafoy lesion was visualized on the greater curvature of the stomach (Figure 3). Three hemostatic clips were successfully placed until hemostasis was achieved. Subsequent mesenteric angiography demonstrated an occlusion of the splenic artery resulting in an enlarged tortuous collateral supply from the left gastric artery, which was determined to be the source of the patient’s bleeding (Figure 4). Embolization of the left gastric artery was then performed, resulting in the complete resolution of the patient’s upper gastrointestinal bleeding.
Discussion: The diagnosis of Dieulafoy lesions can be rather challenging and should be considered on the differential if BRTO fails to control presumed variceal bleeding. Once addressed, mesenteric angiography is recommended if bleeding persists following endoscopic therapy for a Dieulafoy lesion. Although contrast-enhanced CT scans provide some diagnostic utility for gastric varices, endoscopy remains the gold standard for diagnosis. Our case highlights the importance of a thorough endoscopic evaluation prior to diagnosing gastric varices as the true diagnosis could be an obscure Dieulafoy lesion.

Figure: Figure 1: Small <1mm erosion (arrow) present on the lesser curvature of the stomach.
Figure 2: Large blood clot occupying the gastric fundus and body.
Figure 3: Dieulafoy lesion with active extravasation following the placement of two hemostatic clips.
Figure 4: Mesenteric angiography showing an enlarged left gastric artery (arrow).
Figure 2: Large blood clot occupying the gastric fundus and body.
Figure 3: Dieulafoy lesion with active extravasation following the placement of two hemostatic clips.
Figure 4: Mesenteric angiography showing an enlarged left gastric artery (arrow).
Disclosures:
Alexander Carlson indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Elizabeth Gregory indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Alexander M. Carlson, DO, Clive J. Miranda, DO, MS, Elizabeth Z. Gregory, MD, Mayada Ismail, MD. P2075 - Dieulafoy Lesion Masquerading as a Gastric Varix: An Unexpected Finding on Upper Endoscopy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
