Monday Poster Session
Category: GI Bleeding
P2080 - “Remember the Veins of Retzius”. a Case of Bleeding Duodenal Varices Causing a Life-Threatening Upper GI Bleed
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Melissa Matheus, MD
Larkin Community Hospital, Palm Springs Campus
Doral, FL
Presenting Author(s)
Melissa Matheus, MD1, Adam Z. Koller, DO, MS2, Luis Nasiff, MD3, Mihir Brahmbhatt, MD4
1Larkin Community Hospital, Palm Springs Campus, Doral, FL; 2Palmetto General Hospital, Coral Gables, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, Palm Springs Campus, HIaleah, FL
Introduction: Accounting for only 0.4% of cases of variceal bleeding, duodenal varices are a rare cause of massive and fatal upper GI bleeding (UGIB) with mortality as high as 40%. We present a rare case of a life-threatening duodenal variceal bleed.
Case Description/Methods: A 53-year-old male with a history of NHL in remission and alcohol use disorder presented to the ED after a syncopal episode and melena. In the ED, the patient was hemodynamically unstable. Initial laboratory analysis revealed hemoglobin 3.5 mg/dl and lactic acid 7.0 mmol/L. He was admitted to the ICU where a massive transfusion protocol, pantoprazole drip, octreotide drips, and IV antibiotics were initiated. Once stable, the patient underwent upper endoscopy which revealed grade I esophageal varices, gastric fundal varices, and evidence of old blood in the second part of the duodenum with no stigmata of bleeding. Due to an ongoing drop in hemoglobin, CTA of the abdomen/pelvis was obtained demonstrating cirrhosis, partial thrombus of the splenic and intrahepatic portal veins with severe bleeding duodenal varices at the second and third portions of the duodenum. IR performed a transhepatic venogram which showed a partial thrombus of the left hepatic, superior mesenteric, and splenic veins, and large duodenal varices draining to the veins of Retzius. Selective coil embolizations of the duodenal varices were performed. TIPS was not feasible due to unfavorable anatomy, thrombosis, and poor flow. The patient then remained stable post-procedure and was advised to follow up outpatient for a liver transplant.
Discussion: Duodenal varices are a lesser-known cause UGIB due to their low incidence of bleeding but may cause massive life-threatening bleeding. Occurring most often in the setting of decompensated cirrhosis, duodenal varices may be present in extrahepatic portal hypertension secondary to portal, splenic, superior mesenteric, and IVC vein thrombosis or tumor compression. They are often missed endoscopically due to their occult location deep in the serosal layer and variable extension from the first to the fourth portion of the duodenum. Also, varices may become flattened with insufflation and undifferentiable from the duodenal folds. Due to its low incidence of bleeding, studies for the best treatment modality are non-existent. Currently, treatment of duodenal variceal bleeds is based on endoscopist expertise and may include endoscopic sclerotherapy, endoscopic ligation, hemoclips, TIPS, BRTO, IR coiling, and surgery.

Disclosures:
Melissa Matheus, MD1, Adam Z. Koller, DO, MS2, Luis Nasiff, MD3, Mihir Brahmbhatt, MD4. P2080 - “Remember the Veins of Retzius”. a Case of Bleeding Duodenal Varices Causing a Life-Threatening Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Larkin Community Hospital, Palm Springs Campus, Doral, FL; 2Palmetto General Hospital, Coral Gables, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, Palm Springs Campus, HIaleah, FL
Introduction: Accounting for only 0.4% of cases of variceal bleeding, duodenal varices are a rare cause of massive and fatal upper GI bleeding (UGIB) with mortality as high as 40%. We present a rare case of a life-threatening duodenal variceal bleed.
Case Description/Methods: A 53-year-old male with a history of NHL in remission and alcohol use disorder presented to the ED after a syncopal episode and melena. In the ED, the patient was hemodynamically unstable. Initial laboratory analysis revealed hemoglobin 3.5 mg/dl and lactic acid 7.0 mmol/L. He was admitted to the ICU where a massive transfusion protocol, pantoprazole drip, octreotide drips, and IV antibiotics were initiated. Once stable, the patient underwent upper endoscopy which revealed grade I esophageal varices, gastric fundal varices, and evidence of old blood in the second part of the duodenum with no stigmata of bleeding. Due to an ongoing drop in hemoglobin, CTA of the abdomen/pelvis was obtained demonstrating cirrhosis, partial thrombus of the splenic and intrahepatic portal veins with severe bleeding duodenal varices at the second and third portions of the duodenum. IR performed a transhepatic venogram which showed a partial thrombus of the left hepatic, superior mesenteric, and splenic veins, and large duodenal varices draining to the veins of Retzius. Selective coil embolizations of the duodenal varices were performed. TIPS was not feasible due to unfavorable anatomy, thrombosis, and poor flow. The patient then remained stable post-procedure and was advised to follow up outpatient for a liver transplant.
Discussion: Duodenal varices are a lesser-known cause UGIB due to their low incidence of bleeding but may cause massive life-threatening bleeding. Occurring most often in the setting of decompensated cirrhosis, duodenal varices may be present in extrahepatic portal hypertension secondary to portal, splenic, superior mesenteric, and IVC vein thrombosis or tumor compression. They are often missed endoscopically due to their occult location deep in the serosal layer and variable extension from the first to the fourth portion of the duodenum. Also, varices may become flattened with insufflation and undifferentiable from the duodenal folds. Due to its low incidence of bleeding, studies for the best treatment modality are non-existent. Currently, treatment of duodenal variceal bleeds is based on endoscopist expertise and may include endoscopic sclerotherapy, endoscopic ligation, hemoclips, TIPS, BRTO, IR coiling, and surgery.

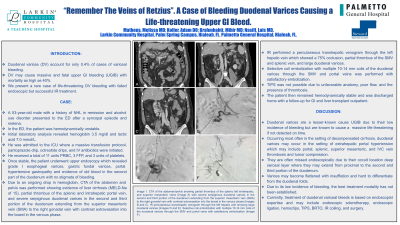
Figure: Image 1. CTA of the abdomen/pelvis showing partial thrombus of the splenic left intrahepatic, and superior mesenteric veins (Image A) with severe serpiginous duodenal varices in the second and third portion of the duodenum extending from the superior mesenteric vein (SMA) to the right gonadal vein with contrast extravasation into the bowel in the venous phase (Images B and C). IR percutaneous transhepatic venogram through the left hepatic vein showing large duodenal varices (Images D and E). Selective coil embolization with multiple 10-14 mm coils of the duodenal varices through the SMV and portal veins with satisfactory embolization (Image F).
Disclosures:
Melissa Matheus indicated no relevant financial relationships.
Adam Koller indicated no relevant financial relationships.
Luis Nasiff indicated no relevant financial relationships.
Mihir Brahmbhatt indicated no relevant financial relationships.
Melissa Matheus, MD1, Adam Z. Koller, DO, MS2, Luis Nasiff, MD3, Mihir Brahmbhatt, MD4. P2080 - “Remember the Veins of Retzius”. a Case of Bleeding Duodenal Varices Causing a Life-Threatening Upper GI Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
